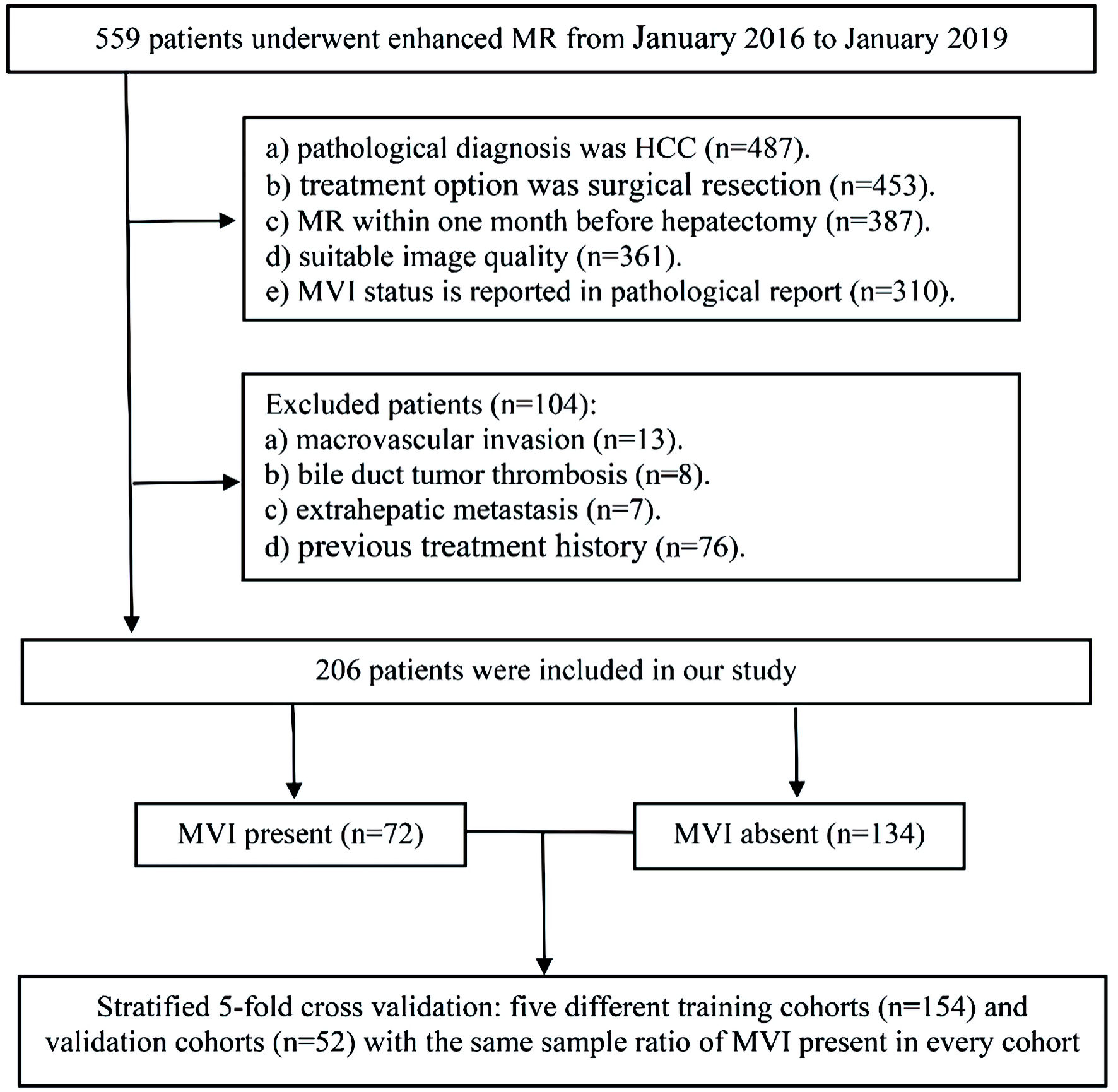
Figure 1. The workflow of patient selection for this study. MR: magnetic resonance; MVI: microvascular invasion; HCC: hepatocellular carcinoma.
| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://www.wjon.org |
Original Article
Volume 15, Number 1, February 2024, pages 58-71
Radiomics of Preoperative Multi-Sequence Magnetic Resonance Imaging Can Improve the Predictive Performance of Microvascular Invasion in Hepatocellular Carcinoma
Figures
Tables
| Characteristic | Total (n = 206) | MVI absent (n = 134) | MVI present (n = 72) | Univariable logistic regression | |
|---|---|---|---|---|---|
| OR (95%CI) | P | ||||
| *P < 0.05. The original units of lg10 converted variables are AFP (ng/L), PIVKA-II (mAU/mL). P is the P value of univariate logistic regression analysis. MVI: microvascular invasion; OR: odd ratio; CI: confidence interval; BCLC: Barcelona Clinic Liver Cancer; HBV: hepatitis B virus; AFP: alpha-fetoprotein; PIVKA-II: protein induced by vitamin K absence or antagonist-II; CA199: carbohydrate antigen 19-9; APHE: arterial phase hyperenhancement; MRI: magnetic resonance imaging. | |||||
| Clinical features | |||||
| Age | 55.19 ± 10.69 | 54.69 ± 10.85 | 56.13 ± 10.38 | 1.013 (0.986, 1.041) | 0.357 |
| Gender | |||||
| Male | 172 (83.5%) | 108 (52.4%) | 64 (31.1%) | ||
| Female | 34 (16.5%) | 26 (12.6%) | 8 (3.9%) | 0.519 (0.222, 1.216) | 0.131 |
| BCLC stage | 0.080 | ||||
| 0 | 52 (25.2%) | 32 (15.5%) | 20 (9.7%) | ||
| A | 139 (67.5%) | 96 (46.6%) | 43 (20.9%) | 0.717 (0.369, 1.393) | 0.326 |
| B | 15 (7.3%) | 6 (2.9%) | 9 (4.4%) | 2.400 (0.742, 7.767) | 0.144 |
| Child-Pugh stage | |||||
| A | 198 (96.1%) | 127 (61.7%) | 71 (34.5%) | ||
| B | 8 (3.9%) | 7 (3.4%) | 1 (0.5%) | 0.256 (0.031, 2.119) | 0.206 |
| Liver disease | |||||
| HBV | 181 (87.9%) | 116 (56.3%) | 65 (31.6%) | ||
| None or other | 25 (12.1%) | 18 (8.7%) | 7 (3.4%) | 0.694 (0.275, 1.749) | 0.439 |
| AFP-L3 | |||||
| Negative | 131 (63.7%) | 87 (42.2%) | 44 (21.4%) | ||
| Positive | 75 (36.4%) | 47 (22.8%) | 28 (13.6%) | 1.178 (0.652, 2.129) | 0.588 |
| AFP_lg10 | 1.47 (0.66 - 2.34) | 1.18 (0.52 - 2.13) | 1.8 (0.99 - 2.65) | 1.607 (1.175, 2.196) | 0.003* |
| PIVKA-II_lg10 | 2.05 (1.52 - 2.79) | 2.03 (1.44 - 2.72) | 2.17 (1.67 - 2.98) | 1.412 (1.004, 1.986) | 0.047* |
| CA199 (U/mL) | 16.45 (8.5 - 28.3) | 17.3 (9.05 - 28.25) | 15.1 (8.05 - 28.5) | 0.992 (0.976, 1.008) | 0.306 |
| HBsAg | |||||
| Negative | 32 (15.5%) | 22 (10.7%) | 10 (4.9%) | ||
| Positive | 174 (84.5%) | 112 (54.4%) | 62 (30.1%) | 1.218 (0.542, 2.736) | 0.633 |
| Pathologic factors | |||||
| Microscopic cirrhosis | |||||
| Absent | 128 (62.1%) | 83 (40.3%) | 45 (21.8%) | ||
| Present | 78 (37.9%) | 51 (24.8%) | 27 (13.1%) | 0.976 (0.541, 1.763) | 0.976 |
| Satellite nodules | |||||
| Absent | 183 (88.8%) | 124 (60.2%) | 59 (28.6%) | ||
| Present | 23 (11.2%) | 10 (4.9%) | 13 (6.3%) | 2.732 (1.132, 6.592) | 0.025* |
| Edmondson-Steiner grade | |||||
| I -II | 26 (12.6%) | 20 (9.7%) | 6 (2.9%) | ||
| III - IV | 180 (87.4%) | 114 (55.3%) | 66 (32%) | 1.930 (0.738, 5.047) | 0.180 |
| MRI features | |||||
| Tumor diameter (cm) | 3 (2.18 - 4.43) | 2.9 (2.2 - 4.13) | 3.45 (2.03 - 5.28) | 1.105 (0.945, 1.293) | 0.212 |
| Tumor number | |||||
| Solitary | 188 (91.3%) | 126 (61.2%) | 62 (30.1%) | ||
| Multiple | 18 (8.7%) | 8 (3.9%) | 10 (4.9%) | 2.540 (0.955, 6.756) | 0.062 |
| Shape | |||||
| Regular | 125 (60.7%) | 89 (43.2%) | 36 (17.5%) | ||
| Irregular | 81 (39.3%) | 45 (21.8%) | 36 (17.5%) | 1.978 (1.102, 3.549) | 0.022* |
| Margin | |||||
| Smooth | 103 (50%) | 78 (37.9%) | 25 (12.1%) | ||
| Non-smooth | 103 (50%) | 56 (27.2%) | 47 (22.8%) | 2.619 (1.445, 4.744) | 0.002* |
| Radiological capsule enhancement | < 0.001* | ||||
| Complete | 79 (38.3%) | 68 (33%) | 11 (5.3%) | ||
| Incomplete | 86 (41.7%) | 44 (21.4%) | 42 (20.4%) | 5.901 (2.747, 12.675) | < 0.001* |
| Absent | 41 (19.9%) | 22 (10.7%) | 19 (9.2%) | 5.339 (2.204, 12.931) | < 0.001* |
| Restricted diffusion | |||||
| Present | 193 (93.7%) | 123 (59.7%) | 70 (34%) | ||
| Absent | 13 (6.3%) | 11 (5.3%) | 2 (1%) | 0.319 (0.069, 1.483) | 0.145 |
| Nonrim APHE | |||||
| Present | 123 (59.7%) | 97 (47.1%) | 26 (12.6%) | ||
| Absent | 83 (40.3%) | 37 (18%) | 46 (22.3%) | 4.638 (2.515, 8.554) | < 0.001* |
| Rim APHE | |||||
| Absent | 136 (66%) | 104 (50.5%) | 32 (15.5%) | ||
| Present | 70 (34%) | 30 (14.6%) | 40 (19.4%) | 4.333 (2.337, 8.034) | < 0.001* |
| Non-peripheral “washout” | |||||
| Present | 123 (59.7%) | 92 (44.7%) | 31 (15 %) | ||
| Absent | 83 (40.3%) | 42 (20.4%) | 41 (19.9%) | 2.897 (1.602, 5.238) | < 0.001* |
| Enhancement pattern | |||||
| Typical | 118 (57.3%) | 91 (44.2%) | 27 (13.1%) | ||
| Atypical | 88 (42.7%) | 43 (20.9%) | 45 (21.8%) | 3.527 (1.937, 6.423) | < 0.001* |
| Arterial peritumoral enhancement | |||||
| Absent | 134 (65%) | 109 (52.9%) | 25 (12.1%) | ||
| Present | 72 (35%) | 25 (12.1%) | 47 (22.8%) | 8.197 (4.273, 15.723) | < 0.001* |
| MRI liver cirrhosis | |||||
| Absent | 57 (27.7%) | 44 (21.4%) | 13 (6.3%) | ||
| Present | 149 (72.3%) | 90 (43.7%) | 59 (28.6%) | 2.219 (1.101, 4.470) | 0.026* |
| Variable | Univariable logistic regression | Multivariable logistic regression | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | |
| P is the P value of univariate and multivariate logistic regression analysis. MVI: microvascular invasion; OR: odd ratio; CI: confidence interval; AFP: alpha-fetoprotein; PIVKA-II: protein induced by vitamin K absence or antagonist-II; APHE: arterial phase hyperenhancement; MRI: magnetic resonance imaging. | ||||||
| AFP_lg10 | 1.607 | 1.175, 2.196 | 0.003 | 1.469 | 1.002, 2.154 | 0.049 |
| PIVKA-II_lg10 | 1.412 | 1.004, 1.986 | 0.047 | |||
| Shape (irregular) | 1.978 | 1.102, 3.549 | 0.022 | |||
| Margin (non-smooth) | 2.619 | 1.445, 4.744 | 0.002 | |||
| Radiological capsule enhancement | < 0.001 | 0.002 | ||||
| Incomplete | 5.901 | 2.747, 12.675 | < 0.001 | 4.101 | 1.721, 9.770 | 0.001 |
| Absent | 5.339 | 2.204, 12.931 | < 0.001 | 5.193 | 1.797, 15.009 | 0.002 |
| Nonrim APHE (absent) | 4.638 | 2.515, 8.554 | < 0.001 | |||
| Rim APHE (present) | 4.333 | 2.337, 8.034 | < 0.001 | |||
| Non-peripheral “washout” (absent) | 2.897 | 1.602, 5.238 | < 0.001 | |||
| Enhancement pattern (atypical) | 3.527 | 1.937, 6.423 | < 0.001 | 2.793 | 1.358, 5.742 | 0.005 |
| Arterial peritumoral enhancement (present) | 8.197 | 4.273, 15.723 | < 0.001 | 8.222 | 3.917, 17.259 | < 0.001 |
| MRI liver cirrhosis (present) | 2.219 | 1.101, 4.470 | 0.026 | |||
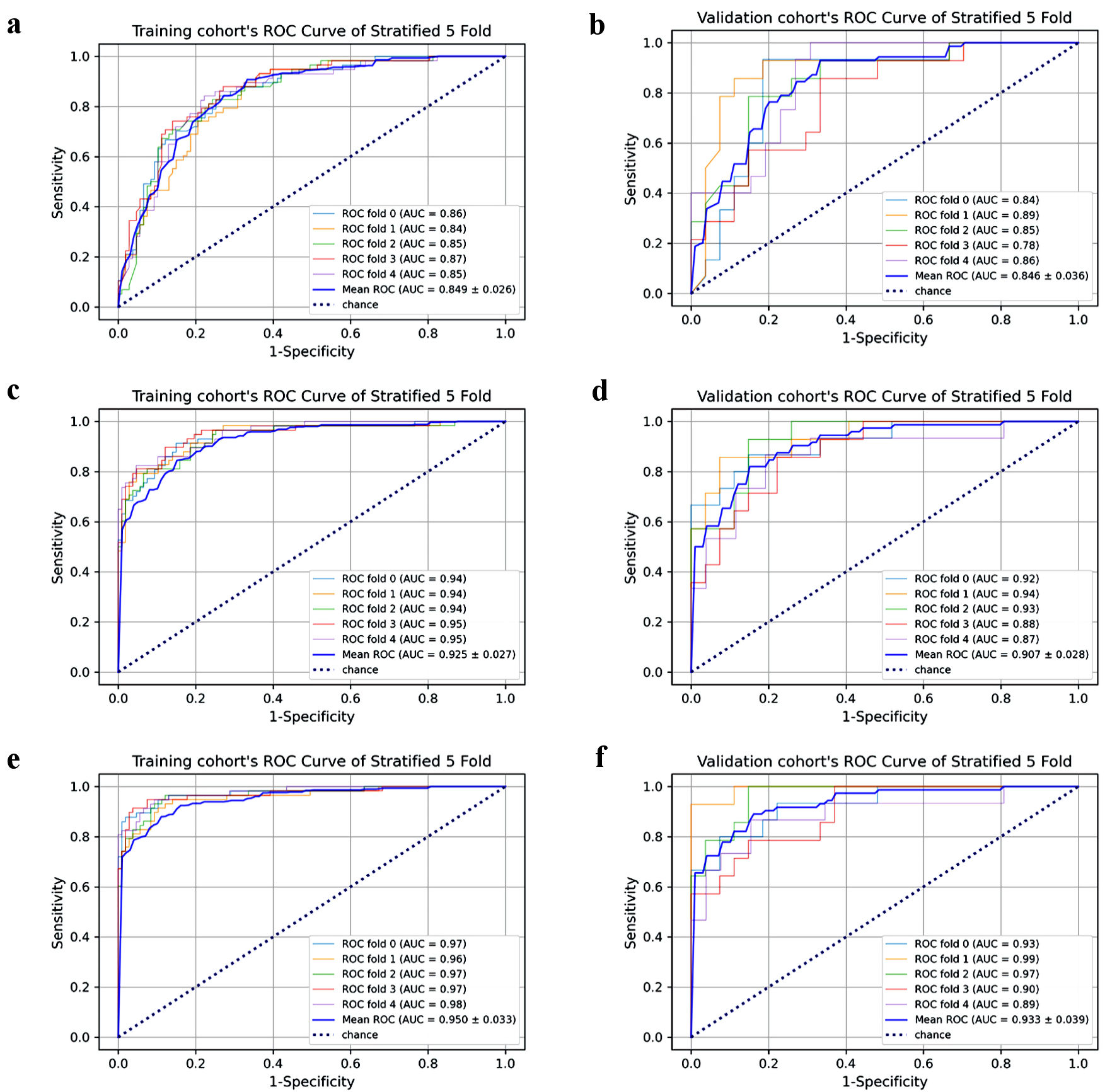
| Sequences (feature number)/model | AUC | f1_score | Accuracy | Sensitivity | Specificity | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Training | Validation | Training | Validation | Training | Validation | Training | Validation | Training | Validation | |
| The training and validation cohort’s performances of each fold for predicting MVI was shown here (Supplementary Material 5, www.wjon.org). ALL = (AP + PP + DP + DWI + T1 + T2), was also the radiomics model. MVI: microvascular invasion; AUC: area under receiver operating characteristic curve; T2: T2-weighted imaging; T1: T1-weighted imaging; DWI: diffusion-weighted imaging; AP: arterial phase; PP: portal phase; DP: delayed phase. | ||||||||||
| AP (20) | 0.842 | 0.805 | 0.721 | 0.624 | 0.825 | 0.767 | 0.667 | 0.610 | 0.848 | 0.838 |
| PP (15) | 0.831 | 0.808 | 0.635 | 0.539 | 0.778 | 0.718 | 0.839 | 0.817 | 0.697 | 0.697 |
| DP (13) | 0.808 | 0.777 | 0.634 | 0.542 | 0.783 | 0.738 | 0.688 | 0.653 | 0.808 | 0.808 |
| DWI (14) | 0.827 | 0.802 | 0.634 | 0.526 | 0.609 | 0.743 | 0.827 | 0.750 | 0.697 | 0.778 |
| T2 (13) | 0.772 | 0.736 | 0.612 | 0.429 | 0.584 | 0.694 | 0.693 | 0.734 | 0.727 | 0.667 |
| T1 (16) | 0.810 | 0.770 | 0.626 | 0.596 | 0.647 | 0.576 | 0.683 | 0.610 | 0.778 | 0.798 |
| AP + DWI (16) | 0.870 | 0.855 | 0.711 | 0.671 | 0.818 | 0.786 | 0.708 | 0.634 | 0.848 | 0.919 |
| AP + PP (17) | 0.855 | 0.819 | 0.746 | 0.616 | 0.842 | 0.762 | 0.673 | 0.628 | 0.889 | 0.889 |
| AP + DP (15) | 0.845 | 0.823 | 0.680 | 0.639 | 0.805 | 0.776 | 0.721 | 0.749 | 0.798 | 0.737 |
| PP + DP (17) | 0.854 | 0.810 | 0.719 | 0.618 | 0.824 | 0.772 | 0.702 | 0.791 | 0.838 | 0.667 |
| PP + DWI (18) | 0.872 | 0.855 | 0.720 | 0.659 | 0.822 | 0.787 | 0.770 | 0.807 | 0.848 | 0.798 |
| T1 + T2 (20) | 0.857 | 0.824 | 0.726 | 0.626 | 0.830 | 0.762 | 0.813 | 0.903 | 0.737 | 0.667 |
| AP + PP + DP (15) | 0.859 | 0.835 | 0.718 | 0.669 | 0.822 | 0.791 | 0.727 | 0.791 | 0.838 | 0.737 |
| AP + PP + DWI (19) | 0.889 | 0.860 | 0.783 | 0.656 | 0.858 | 0.777 | 0.857 | 0.834 | 0.778 | 0.768 |
| AP + DP + DWI (20) | 0.916 | 0.897 | 0.809 | 0.788 | 0.876 | 0.859 | 0.803 | 0.790 | 0.889 | 0.889 |
| PP + DP + DWI (20) | 0.906 | 0.878 | 0.810 | 0.712 | 0.881 | 0.815 | 0.813 | 0.831 | 0.848 | 0.778 |
| AP + PP + DP + DWI (20) | 0.920 | 0.904 | 0.829 | 0.707 | 0.888 | 0.811 | 0.824 | 0.790 | 0.889 | 0.879 |
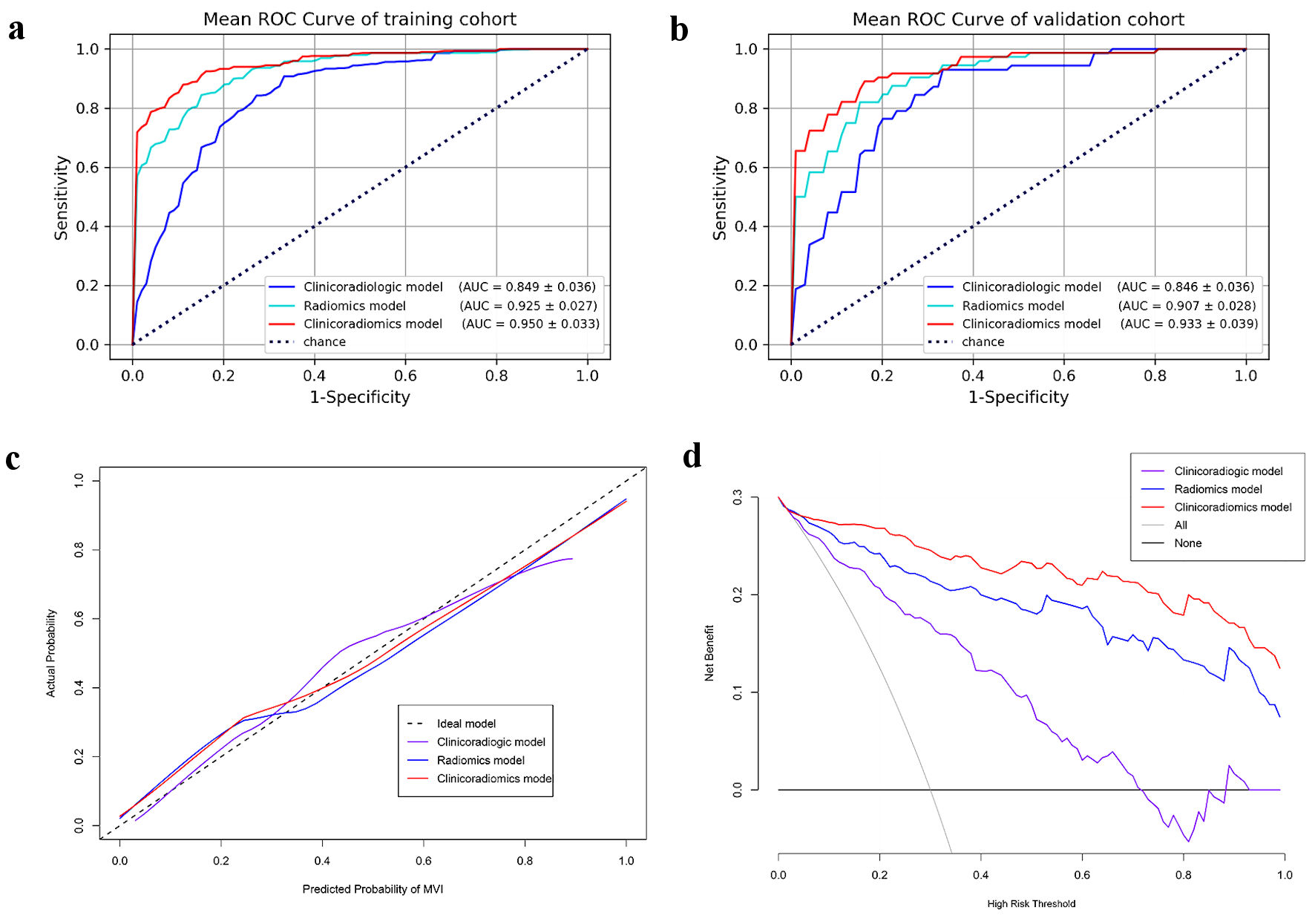
| ALL/radiomics (18) | 0.925 | 0.907 | 0.823 | 0.722 | 0.883 | 0.820 | 0.844 | 0.820 | 0.848 | 0.848 |
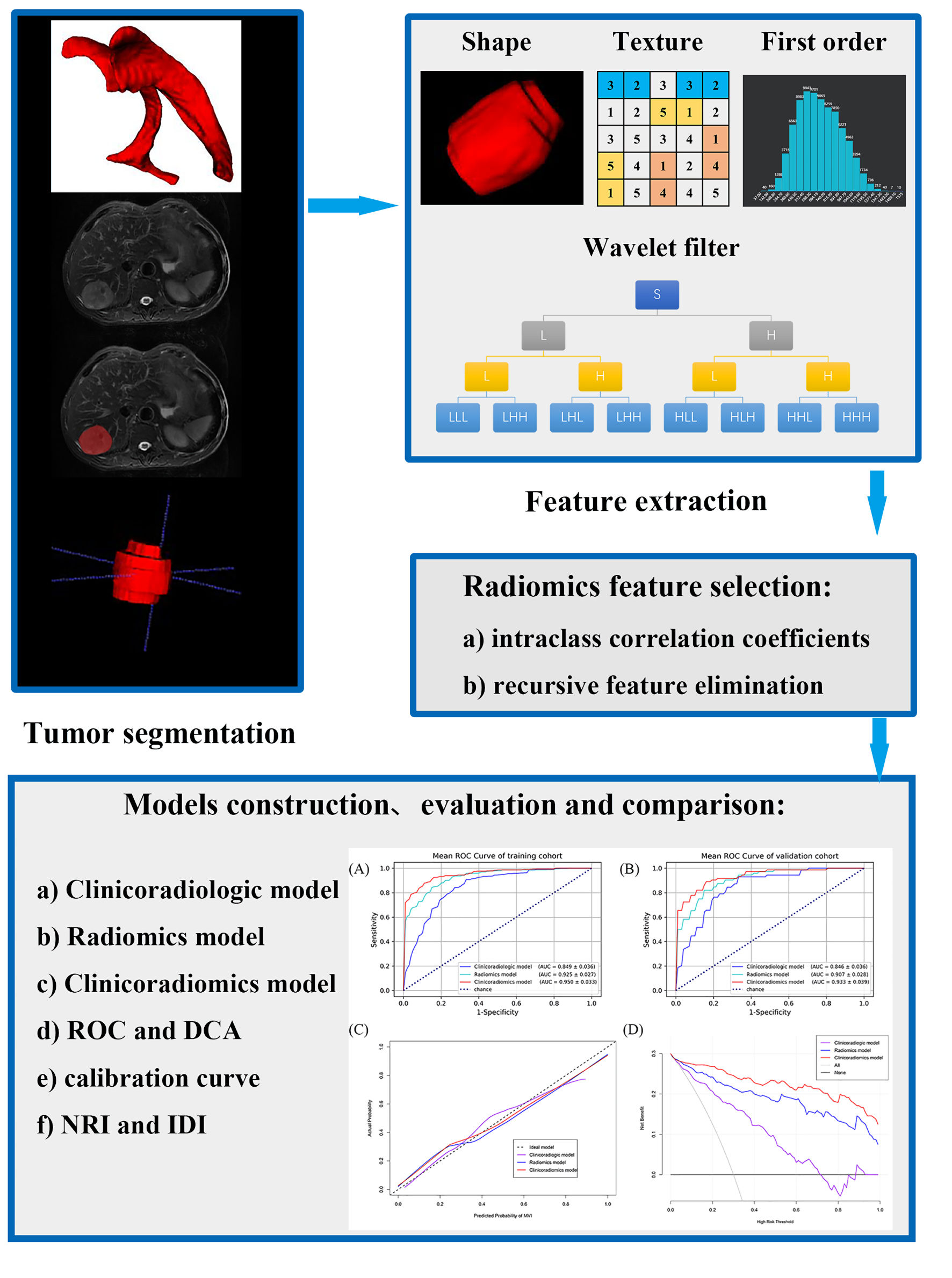
| Clinicoradiologic | 0.849 | 0.846 | 0.643 | 0.576 | 0.779 | 0.743 | 0.843 | 0.930 | 0.727 | 0.667 |
| Clinicoradiomics | 0.950 | 0.933 | 0.887 | 0.812 | 0.779 | 0.869 | 0.879 | 0.890 | 0.889 | 0.838 |
| P (AUC) | NRI | P (NRI) | IDI | P (IDI) | |
|---|---|---|---|---|---|
| P is the probability when Delong test is used to compare the ROC curve of two models. AUC: area under receiver operating characteristic curve; NRI: net reclassification improvement; IDI: integrated discrimination improvement. | |||||
| Radiomics vs. clinicoradiologic | 0.0017 | 0.575 | 0.0014 | 0.280 | < 0.05 |
| Clinicoradiomics vs. clinicoradiologic | < 0.0001 | 0.825 | < 0.0001 | 0.398 | < 0.05 |
| Clinicoradiomics vs. radiomics | 0.0122 | 0.313 | 0.0085 | 0.117 | < 0.05 |