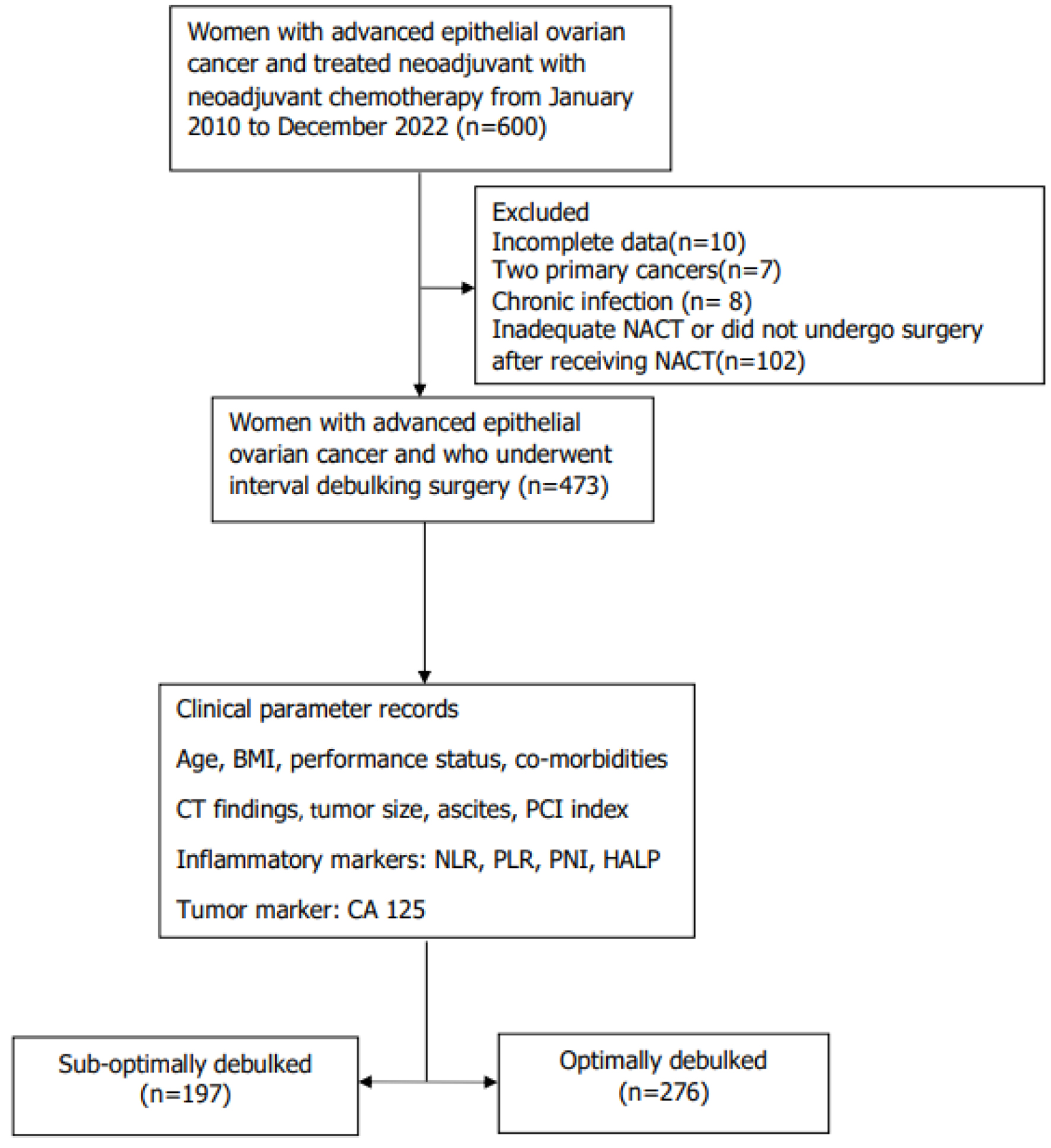
Figure 1. Flow chart of patients within the study. BMI: body mass index; ECOG: Eastern Cooperative Oncology Group; FIGO: International Federation of Gynecology and Obstetrics; HALP: hemoglobin-albumin-lymphocyte-platelet; IDS: interval debulking surgery; NACT: neoadjuvant chemotherapy; NLR: neutrophil-to-lymphocyte ratio; PLR: platelet-to-lymphocyte ratio; PNI: prognostic nutritional index.