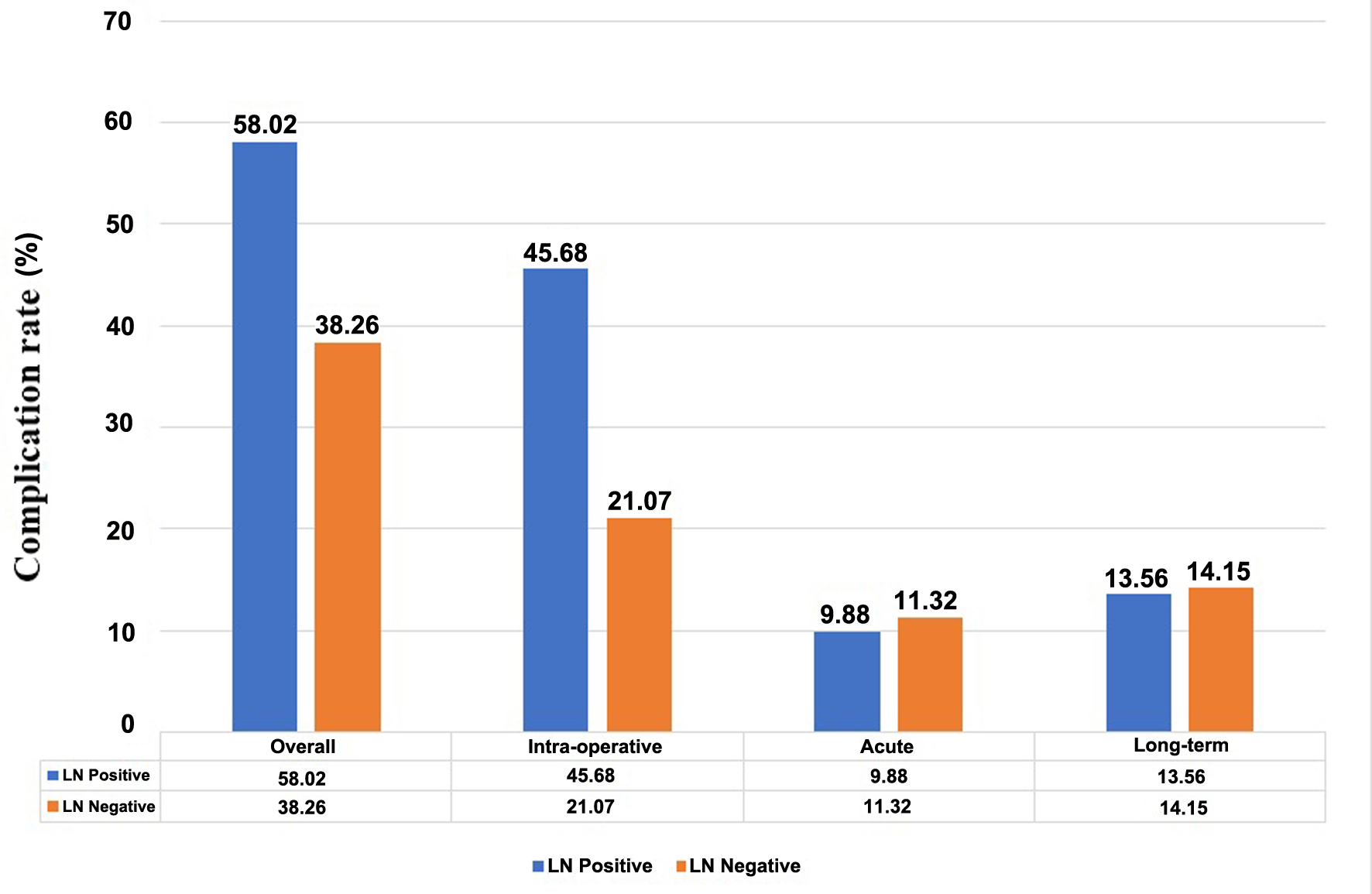
Figure 1. Complication rate of subgroup of patients with or without lymph node metastasis.
| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://www.wjon.org |
Original Article
Volume 15, Number 3, June 2024, pages 423-431
A Retrospective Study of Complications Following Pelvic and Para-Aortic Lymphadenectomy in Gynecologic Oncology
Figures
Tables
| Characteristics | Mean ± SD or N (%) |
|---|---|
| BMI: body mass index; SD: standard deviation. | |
| Age (years) | 53.7 ± 12.4 |
| BMI (kg/m2) | 25.8 ± 5.8 |
| 25 - 29.9 | 118 (29.6) |
| 30 - 39.9 | 65 (16.3) |
| ≥ 40 | 11 (2.8) |
| Underlying disease | |
| No | 160 (40.1) |
| Yes | 239 (59.9) |
| Diabetes mellitus | 85 (21.3) |
| Hypertension | 143 (35.8) |
| Dyslipidemia | 94 (23.6) |
| Cerebrovascular accident | 7 (1.8) |
| Cardiovascular disease | 5 (1.3) |
| Venous thromboembolism | 13 (3.3) |
| Hyperthyroidism | 8 (2.0) |
| Hypothyroidism | 7 (1.8) |
| HIV infection | 7 (1.8) |
| Obstructive sleep apnea | 5 (1.3) |
| Gynecologic cancers | |
| Cervical cancer | 81 (20.3) |
| Endometrial cancer | 174 (43.6) |
| Ovarian cancer | 140 (35.1) |
| Synchronous cancer | 4 (1.0) |
| Total (N = 399) | Types of cancer | ||||
|---|---|---|---|---|---|
| Cervix (N = 81) | Endometrium (N = 174) | Ovary (N = 140) | Synchronousa (N = 4) | ||
| aSynchronous cancer: ovarian cancer with endometrium cancer in four cases. bType 2 or 3 hysterectomy. BSO: bilateral salpingo-oophorectomy; LN: lymph node; SD: standard deviation; USO: unilateral salpingo-oophorectomy. | |||||
| Surgical approach (%) | |||||
| Laparotomy | 354 (88.7) | 73 (90.1) | 139 (79.9) | 138 (98.6) | 4 (100.0) |
| Laparoscopy | 45 (11.3) | 8 (9.9) | 35 (20.1) | 2 (1.4) | 0 (0.0) |
| Lymphadenectomy (%) | |||||
| Pelvic lymphadenectomy | 103 (25.8) | 66 (81.5) | 22 (12.6) | 15 (10.7) | 0 (0.0) |
| Para-aortic lymphadenectomy | 5 (1.3) | 4 (4.9) | 1 (0.6) | 0 (0.0) | 0 (0.0) |
| Pelvic and para-aortic lymphadenectomy | 291 (72.9) | 11 (13.6) | 151 (86.8) | 125 (89.3) | 4 (100.0) |
| Operations (%) | |||||
| Hysterectomy (± BSO ± omentectomy) | 372 (93.2) | 72 (88.9)b | 171 (98.3) | 125 (89.3) | 4 (100.0) |
| USO/BSO (± omentectomy) | 13 (3.3) | 0 (0.0) | 1 (0.6) | 12 (8.6) | 0 (0.0) |
| Other operations | 8 (2.0) | 4 (4.9) | 1 (0.6) | 3 (2.1) | 0 (0.0) |
| Lymphadenectomy alone | 6 (1.5) | 5 (6.2) | 1 (0.6) | 0 (0.0) | 0 (0.0) |
| Operative time (min) (mean ± SD) | 273.9 ± 88.2 | 275.0 ± 81.3 | 259.6 ± 79.3 | 293.2 ± 98.5 | 197.5 ± 74.1 |
| Total blood loss (mL) (mean ± SD) | 689.7 ± 757.3 | 559.3 ± 416.5 | 432.4 ± 428.5 | 1,077.1 ± 1,033.0 | 962.5 ± 363.7 |
| Total number of LN (mean ± SD) | 20.4 ± 10.3 | 19.7 ± 10.6 | 21.1 ± 10.7 | 19.7 ± 9.5 | 27.5 ± 10.1 |
| LN status (%) | |||||
| Negative | 318 (79.7) | 69 (85.2) | 143 (82.2) | 102 (72.9) | 4 (100.0) |
| Positive | 81 (20.3) | 12 (14.8) | 31 (17.8) | 38 (27.1) | 0 (0.0) |
| Overall complication (%) | 169 (42.4) | 32 (39.5) | 52 (29.9) | 83 (59.3) | 2 (50.0) |
| Intra-operative complication (%) | 104 (26.1) | 16 (19.8) | 22 (12.6) | 65 (46.4) | 1 (25.0) |
| Vessel injury | 13 (3.3) | 0 (0.0) | 6 (3.4) | 7 (5.0) | 0 (0.0) |
| Bowel injury | 13 (3.3) | 1 (1.2) | 3 (1.7) | 9 (6.4) | 0 (0.0) |
| Bladder injury | 5 (1.3) | 0 (0.0) | 1 (0.6) | 4 (2.9) | 0 (0.0) |
| Ureteric injury | 3 (0.8) | 1 (1.2) | 0 (0.0) | 2 (1.4) | 0 (0.0) |
| Blood loss ≥ 1,000 mL | 83 (20.3) | 15 (18.5) | 15 (8.6) | 52 (37.1) | 1 (25.0) |
| Acute post-operative complication (%) | 44 (11.0) | 8 (9.9) | 17 (9.8) | 19 (13.6) | 0 (0.0) |
| Surgical site infection | 16 (4.0) | 1 (1.2) | 10 (5.7) | 5 (3.6) | 0 (0.0) |
| Urinary retention | 3 (0.8) | 3 (3.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Bowel obstruction | 3 (0.8) | 0 (0.0) | 0 (0.0) | 3 (2.1) | 0 (0.0) |
| Bowel ileus | 8 (2.0) | 1 (1.2) | 3 (1.7) | 4 (2.9) | 0 (0.0) |
| Cystitis | 6 (1.5) | 1 (1.2) | 3 (1.7) | 2 (1.4) | 0 (0.0) |
| Lymphocele | 4 (1.0) | 0 (0.0) | 0 (0.0) | 4 (2.9) | 0 (0.0) |
| Venous thromboembolism | 3 (0.8) | 2 (2.5) | 0 (0.0) | 1 (0.7) | 0 (0.0) |
| Hospital acquired pneumonia | 2 (0.5) | 0 (0.0) | 1 (0.6) | 1 (0.7) | 0 (0.0) |
| Long-term complication (%) | 56 (14.0) | 13 (16.0) | 21 (12.1) | 21 (15.0) | 1 (25.0) |
| Lymphedema | 8 (2.0) | 2 (2.5) | 4 (2.3) | 2 (1.4) | 0 (0.0) |
| Lymphocele | 24 (6.0) | 3 (3.7) | 7 (4.0) | 14 (10.0) | 0 (0.0) |
| Venous thromboembolism | 12 (3.0) | 3 (3.7) | 8 (4.6) | 1 (0.7) | 0 (0.0) |
| Urinary retention | 3 (0.8) | 3 (3.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Others (bowel obstruction, vaginal stump evisceration, cystocele) | 11 (2.8) | 2 (2.5) | 4 (2.3) | 4 (2.9) | 1 (25.0) |
| 5-year survival rate (%) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
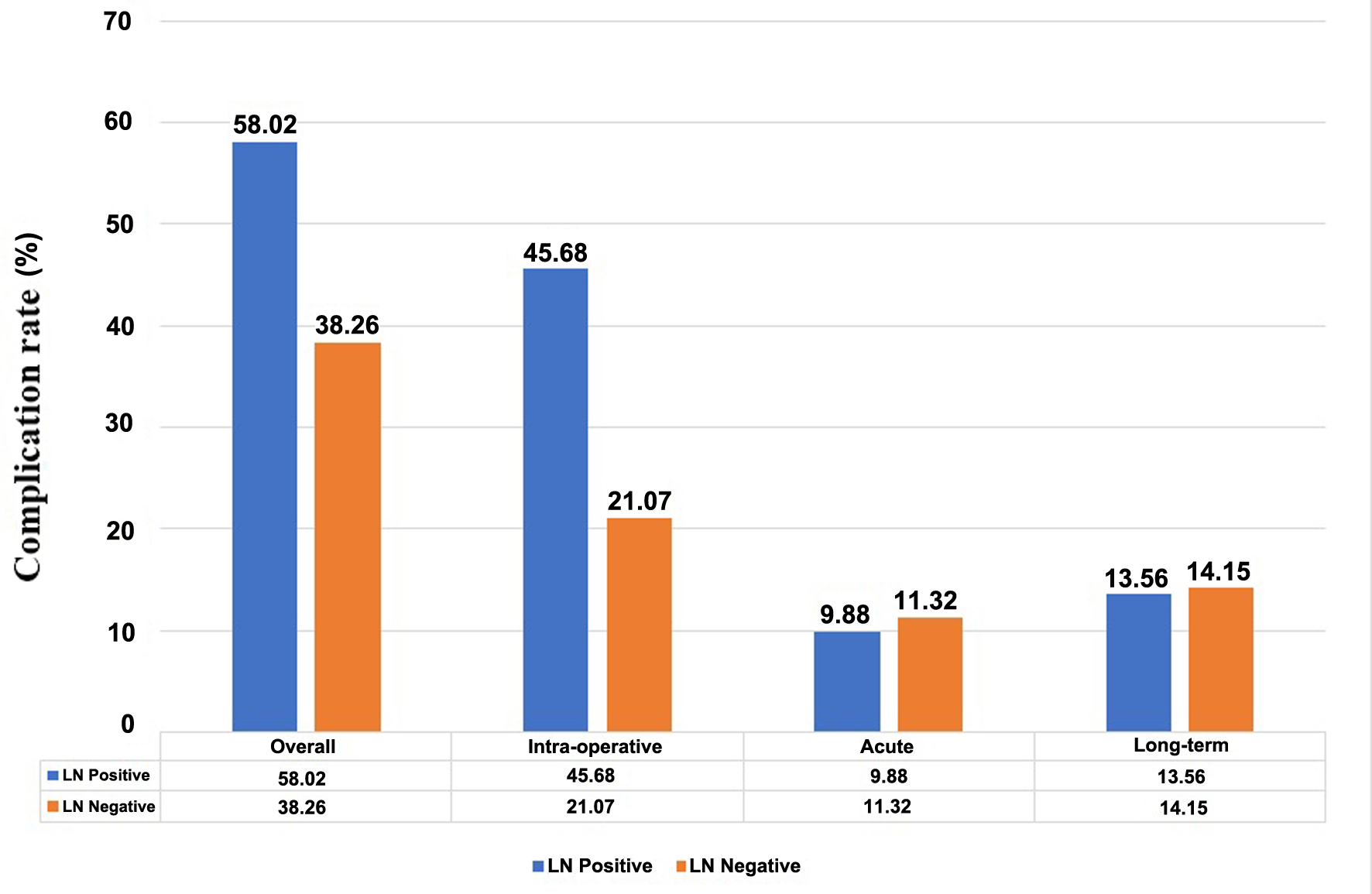
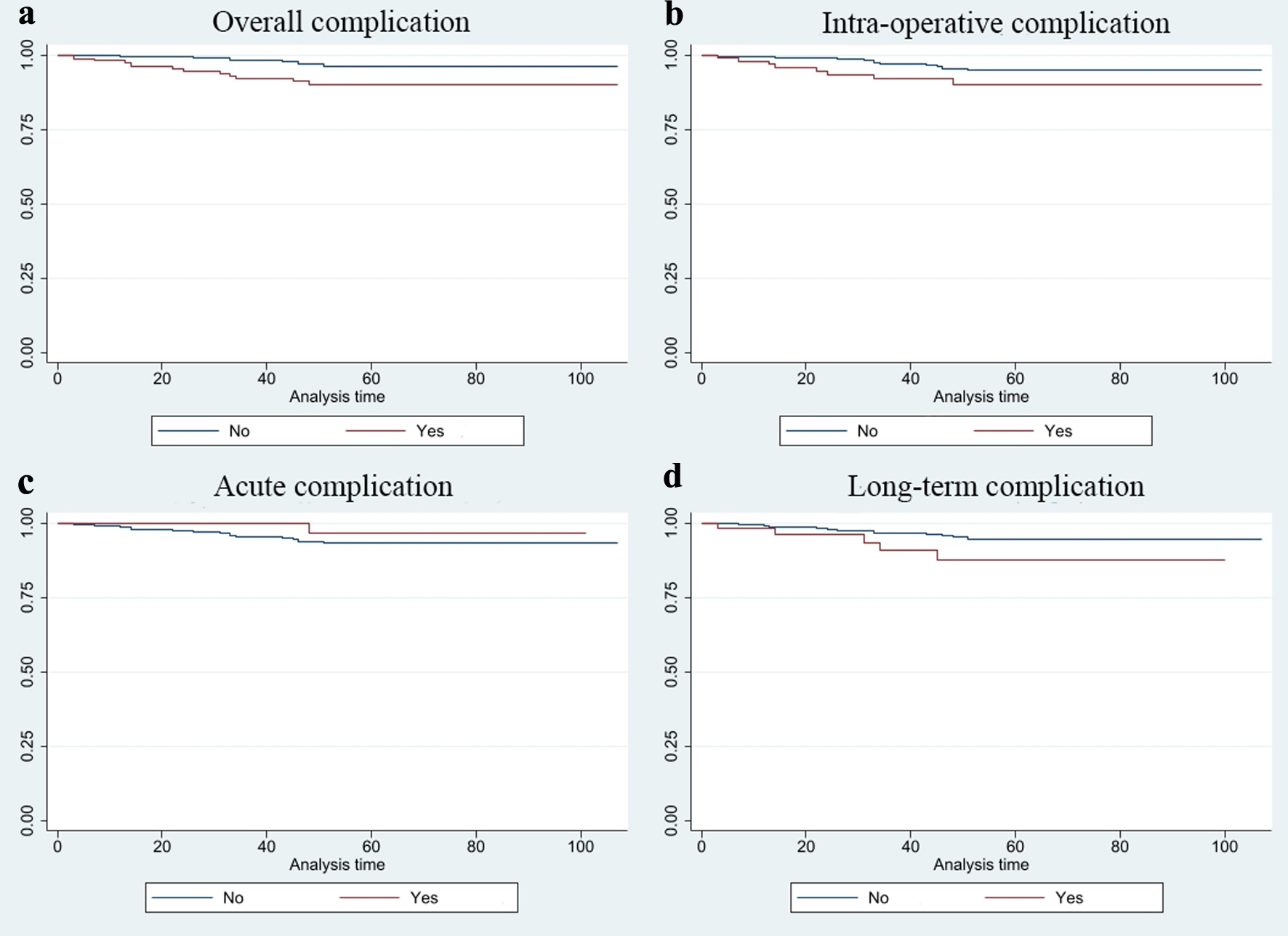
| Overall complication | Intra-operative complication | Acute complication | Long-term complication | |||||||||
| No | Yes | P-value | No | Yes | P-value | No | Yes | P-value | No | Yes | P-value | |
| LN: lymph node. | ||||||||||||
| All patients | 97.39 | 92.31 | 0.017 | 96.27 | 92.31 | 0.080 | 94.93 | 97.73 | 0.3892 | 95.92 | 91.07 | 0.077 |
| Positive LN | 100.00 | 97.87 | 0.221 | 100.00 | 97.30 | 0.089 | 98.63 | 100 | 0.719 | 98.57 | 100.00 | 0.719 |
| Negative LN | 96.94 | 90.16 | 0.030 | 95.62 | 89.55 | 0.163 | 93.97 | 97.22 | 0.424 | 92.49 | 88.89 | 0.058 |