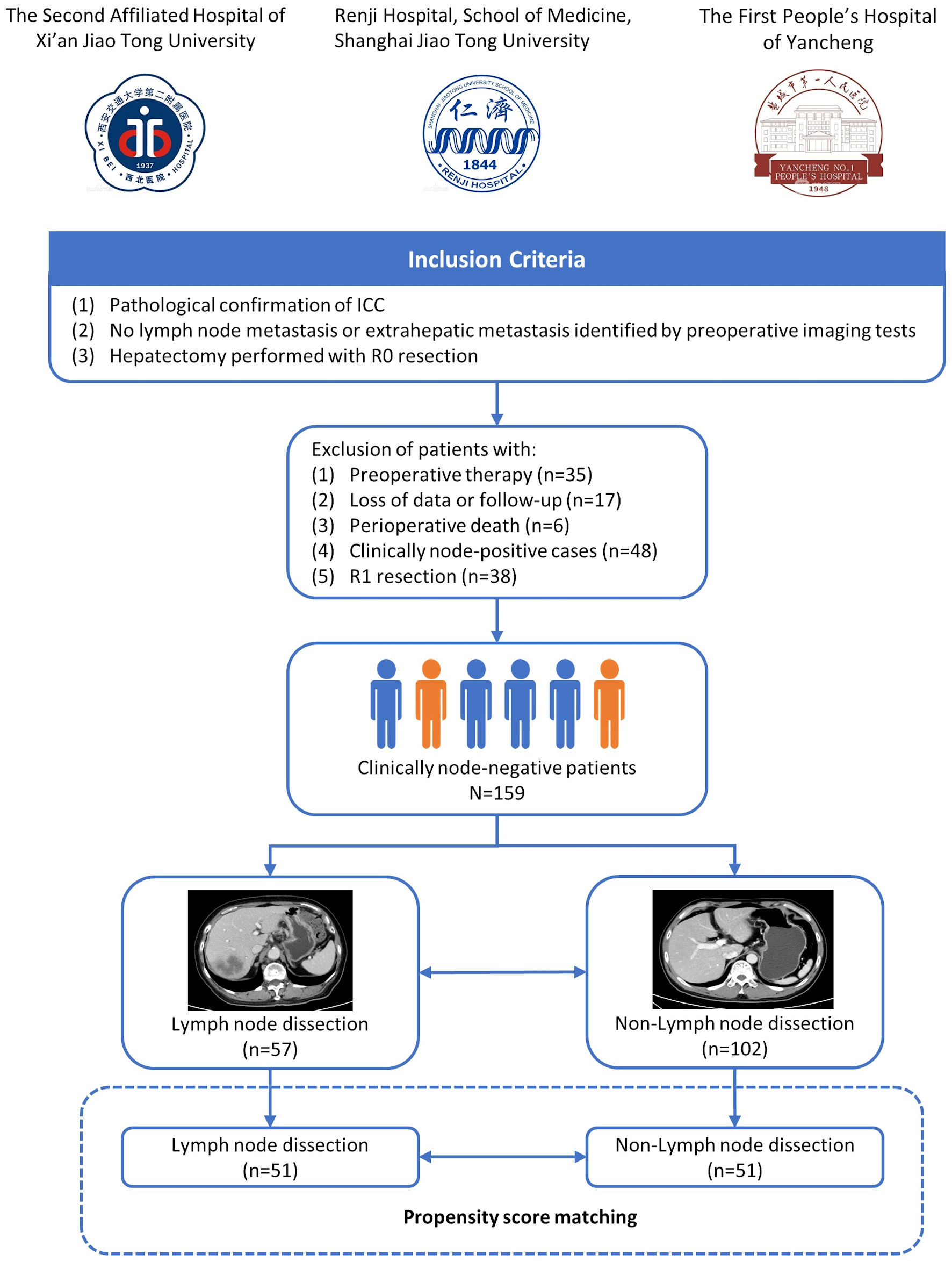
Figure 1. Flowchart of patients’ enrollment. ICC: intrahepatic cholangiocarcinoma.
| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://www.wjon.org |
Original Article
Volume 15, Number 4, August 2024, pages 579-591
Impact of Lymph Node Dissection for Patients With Clinically Node-Negative Intrahepatic Cholangiocarcinoma: A Multicenter Cohort Study
Figures
Tables
| Characteristics | Before PSM | After PSM | ||||
|---|---|---|---|---|---|---|
| Non-LND (n = 102) | LND (n = 57) | P value | Non-LND (n = 51) | LND (n = 51) | P value | |
| P values were calculated using Chi-square test for categorical variables. PSM: propensity score matching; LND: lymph node dissection; KPS: Karnofsky Performance Status; HBV: hepatitis B virus; CA 19-9: carbohydrate antigen 19-9. | ||||||
| Gender | ||||||
| Female | 39 (38.2%) | 19 (33.3%) | 0.538 | 17 (33.3%) | 17 (33.3%) | 1.000 |
| Male | 63 (61.8%) | 38 (66.7%) | 34 (66.7%) | 34 (66.7%) | ||
| Age | ||||||
| ≤ 50 years | 18 (17.6%) | 13 (22.8%) | 0.431 | 13 (25.5%) | 11 (21.6%) | 0.641 |
| > 50 years | 84 (82.4%) | 44 (77.2%) | 38 (74.5%) | 40 (78.4%) | ||
| HBV infection | ||||||
| Absent | 65 (63.7%) | 43 (75.4%) | 0.129 | 39 (76.5%) | 37 (72.5%) | 0.650 |
| Present | 37 (36.3%) | 14 (24.6%) | 12 (23.5%) | 14 (27.5%) | ||
| KPS score | ||||||
| > 60 | 88 (86.3%) | 50 (87.7%) | 0.796 | 43 (84.3%) | 45 (88.2%) | 0.565 |
| ≤ 60 | 14 (13.7%) | 7 (12.3%) | 8 (15.7%) | 6 (11.8%) | ||
| Cirrhosis | ||||||
| Absent | 74 (72.5%) | 55 (96.5%) | < 0.001 | 48 (94.1%) | 49 (96.1%) | 0.647 |
| Present | 28 (27.5%) | 2 (3.5%) | 3 (5.9%) | 2 (3.9%) | ||
| CA 19-9 level | ||||||
| ≤ 55 U/mL | 54 (52.9%) | 30 (52.6%) | 0.970 | 26 (51.0%) | 27 (52.9%) | 0.843 |
| > 55 U/mL | 48 (47.1%) | 27 (47.4%) | 25 (49.0%) | 24 (47.1%) | ||
| Tumor diameter | ||||||
| ≤ 5 cm | 59 (57.8%) | 27 (47.4%) | 0.204 | 22 (43.1%) | 23 (45.1%) | 0.842 |
| > 5 cm | 43 (42.2%) | 30 (52.6%) | 29 (56.9%) | 28 (54.9%) | ||
| Tumor number | ||||||
| Single | 84 (82.4%) | 45 (78.9%) | 0.599 | 40 (78.4%) | 42 (82.4%) | 0.618 |
| Multiple | 18 (17.6%) | 12 (21.1%) | 11 (21.6%) | 9 (17.6%) | ||
| Vascular invasion | ||||||
| Absent | 76 (74.5%) | 35 (61.4%) | 0.084 | 36 (70.6%) | 34 (66.7%) | 0.670 |
| Present | 26 (25.5%) | 22 (38.6%) | 15 (29.4%) | 17 (33.3%) | ||
| Differentiation | ||||||
| Well and moderate | 51 (50.0%) | 36 (63.2%) | 0.110 | 30 (58.8%) | 32 (62.7%) | 0.685 |
| Poor | 51 (50.0%) | 21 (36.8%) | 21 (41.2%) | 19 (37.3%) | ||
| Perineural invasion | ||||||
| Absent | 84 (82.4%) | 51 (89.5%) | 0.229 | 47 (92.2%) | 45 (88.2%) | 0.505 |
| Present | 18 (17.6%) | 6 (10.5%) | 4 (7.8%) | 6 (11.8%) | ||
| Postoperative adjuvant therapy | ||||||
| Absent | 55 (53.9%) | 29 (50.9%) | 0.712 | 29 (56.9%) | 28 (54.9%) | 0.842 |
| Present | 47 (46.1%) | 28 (49.1%) | 22 (43.1%) | 23 (45.1%) | ||
| Characteristics | Before PSM | After PSM | ||||
|---|---|---|---|---|---|---|
| Non-LND (n = 102) | LND (n = 57) | P value | Non-LND (n = 51) | LND (n = 51) | P value | |
| Data were median (interquartile range) and n (%) for continuous and categorical variables. P values were calculated using nonparametric test and Chi-square test for continuous and categorical variables. PSM: propensity score matching; LND: lymph node dissection. | ||||||
| Surgical time (min) | 160 (100, 180) | 160 (120, 190) | 0.319 | 180 (140, 200) | 170 (130, 200) | 0.521 |
| Blood loss (mL) | 200 (50, 300) | 200 (100, 300) | 0.752 | 200 (100, 300) | 200 (100, 200) | 0.454 |
| Postoperative hospital stays (days) | 9 (7, 11) | 10 (8, 12) | 0.021 | 9 (8, 11) | 10 (8, 13) | 0.049 |
| Major complications | 13 (12.7%) | 8 (14.0%) | 0.818 | 8 (15.7%) | 7 (13.7%) | 0.780 |
| Postoperative adjuvant therapy | 47 (46.1%) | 28 (49.1%) | 0.712 | 22 (43.1%) | 23 (45.1%) | 0.842 |
| Characteristics | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P value | HR | 95% CI | P value | |
| KPS: Karnofsky Performance Status; HBV: hepatitis B virus; CA19-9: carbohydrate antigen 19-9; HR: hazard ratio; CI: confidence interval. | ||||||
| Age (≤ 50 vs. > 50) | 1.608 | 0.914 - 2.830 | 0.099 | |||
| Gender (male vs. female) | 1.491 | 0.913 - 2.437 | 0.111 | |||
| HBV infection (absent vs. present) | 0.807 | 0.471 - 1.384 | 0.436 | |||
| KPS score (> 60 vs. ≤ 60) | 1.509 | 0.758 - 2.618 | 0.278 | |||
| Cirrhosis (absent vs. present) | 1.576 | 0.574 - 4.326 | 0.377 | |||
| Preoperative CA19-9 (U/mL) (≤ 55 vs. > 55) | 1.187 | 0.759 - 1.858 | 0.452 | |||
| Tumor diameter (≤ 50 mm vs. > 50 mm) | 2.353 | 1.461 - 3.789 | < 0.001 | 2.027 | 1.231 - 3.338 | 0.005 |
| Tumor number (single vs. multiple) | 1.754 | 1.018 - 3.021 | 0.043 | 1.493 | 0.860 - 2.591 | 0.154 |
| Vascular invasion (absent vs. present) | 1.772 | 1.110 - 2.827 | 0.016 | 1.517 | 0.940 - 2.447 | 0.088 |
| Histologic differentiation (well/moderate vs. poor) | 1.465 | 0.930 - 2.309 | 0.100 | |||
| Perineural invasion (absent vs. present) | 1.386 | 0.690 - 2.784 | 0.358 | |||
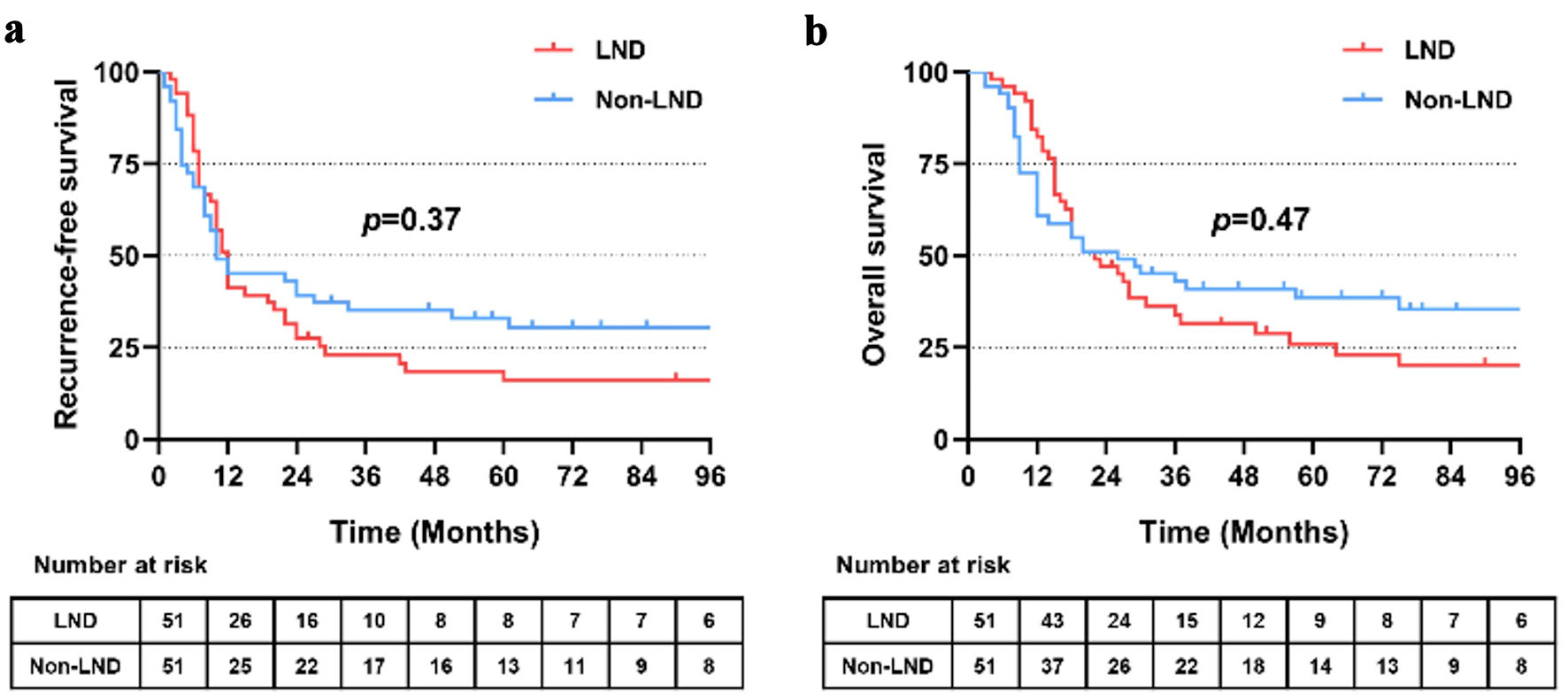
| Lymph node dissection (absent vs. present) | 1.222 | 0.778 - 1.919 | 0.385 | |||
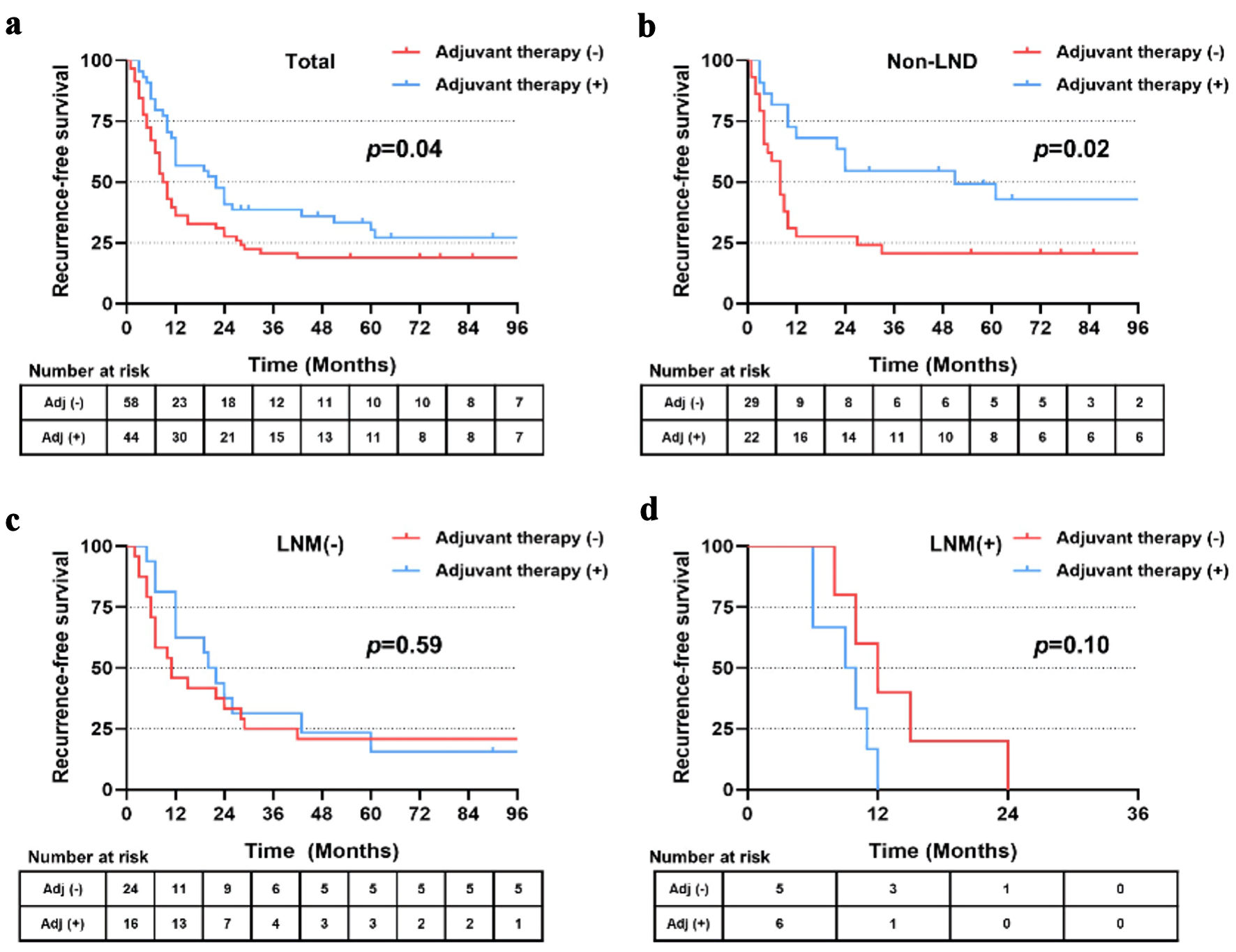
| Postoperative adjuvant therapy (absent vs. present) | 0.619 | 0.392 - 0.978 | 0.040 | 0.623 | 0.393 - 0.987 | 0.044 |
| Characteristics | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P value | HR | 95% CI | P value | |
| KPS: Karnofsky Performance Status; HBV: hepatitis B virus; CA19-9: carbohydrate antigen 19-9; HR: hazard ratio; CI: confidence interval. | ||||||
| Age (≤ 50 vs. > 50) | 1.863 | 1.000 - 3.471 | 0.050 | |||
| Gender (male vs. female) | 1.360 | 0.818 - 2.262 | 0.236 | |||
| HBV infection (absent vs. present) | 0.826 | 0.466 - 1.462 | 0.511 | |||
| KPS score (> 60 vs. ≤ 60) | 1.692 | 0.923 - 3.100 | 0.089 | |||
| Cirrhosis (absent vs. present) | 1.865 | 0.675 - 5.151 | 0.229 | |||
| Preoperative CA19-9 (U/mL) (≤ 55 vs. > 55) | 1.342 | 0.838 - 2.149 | 0.221 | |||
| Tumor diameter (≤ 50 vs. > 50 mm) | 2.383 | 1.443 - 3.936 | 0.001 | 2.172 | 1.304 - 3.618 | 0.003 |
| Tumor number (single vs. multiple) | 2.330 | 1.349 - 4.022 | 0.002 | 2.130 | 1.223 - 3.711 | 0.008 |
| Vascular invasion (absent vs. present) | 1.389 | 0.841 - 2.295 | 0.199 | |||
| Histologic differentiation (well/moderate vs. poor) | 1.605 | 0.997 - 2.583 | 0.051 | |||
| Perineural invasion (absent vs. present) | 1.527 | 0.757 - 3.082 | 0.237 | |||
| Lymph node dissection (absent vs. present) | 1.189 | 0.740 - 1.909 | 0.474 | |||
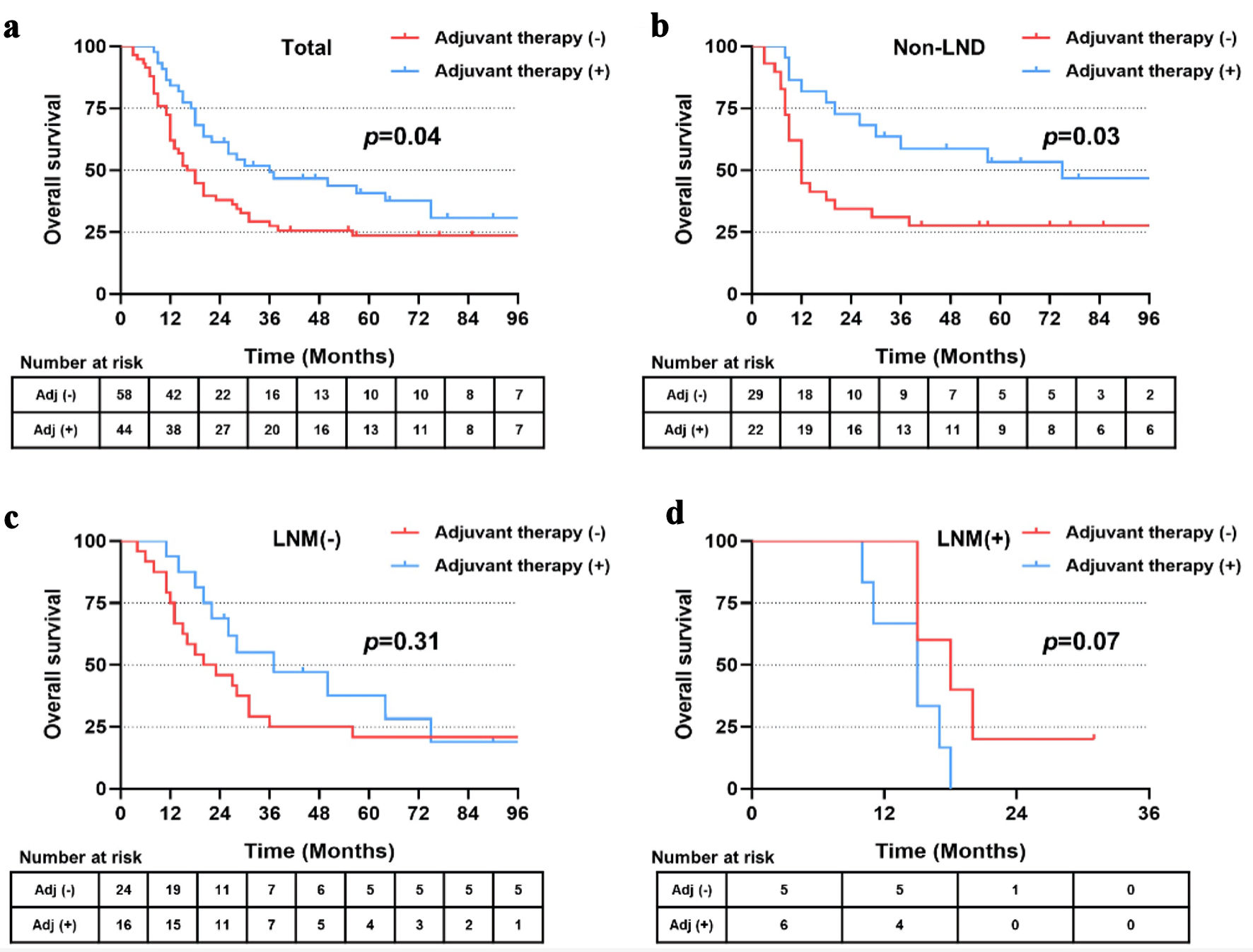
| Postoperative adjuvant therapy (absent vs. present) | 0.578 | 0.357 - 0.936 | 0.026 | 0.585 | 0.359 - 0.952 | 0.031 |