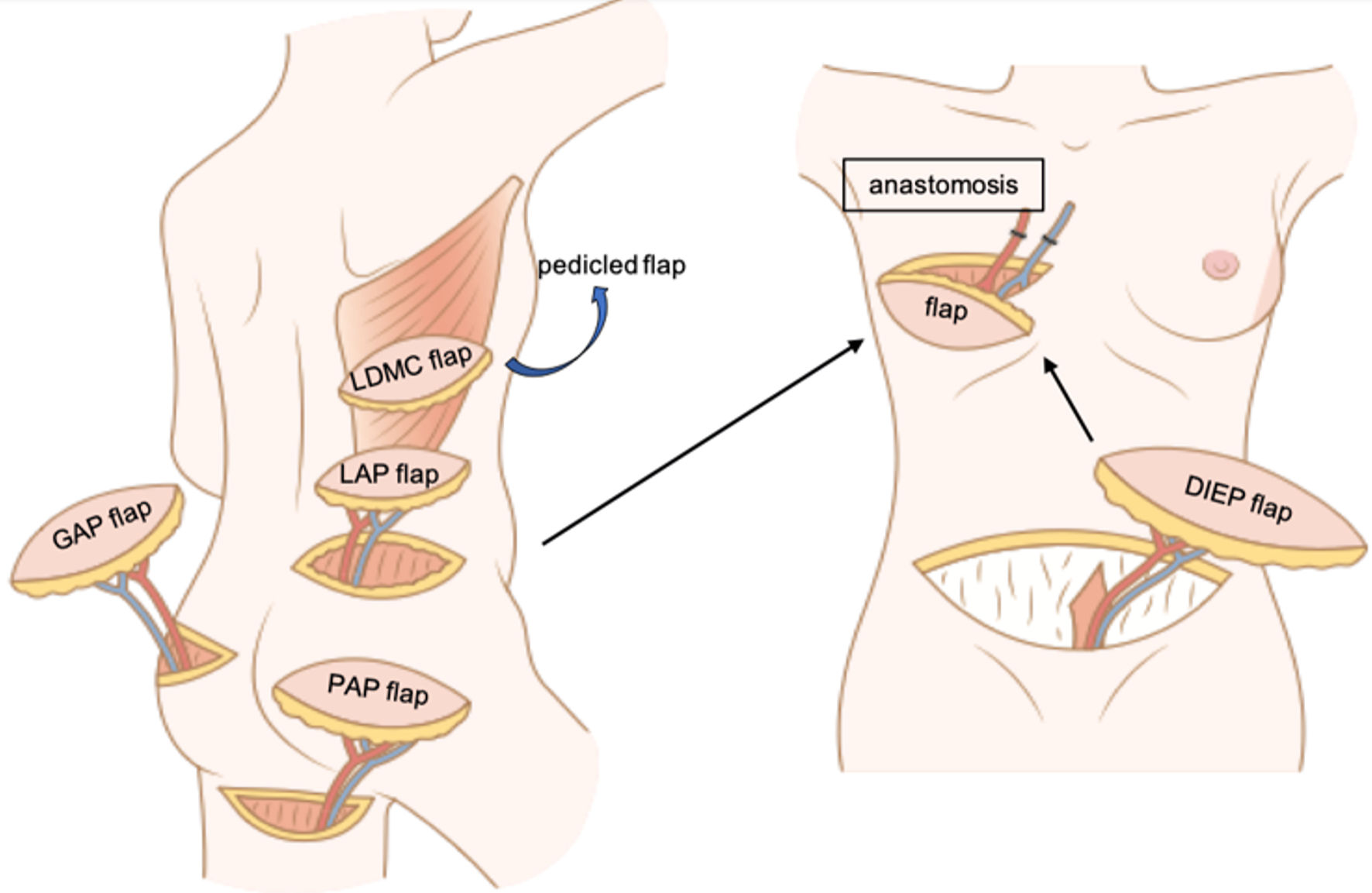
| Flap name | LDMC flap [66] | LAP flap [58] | DIEP flap [68] | TRAM flap [69] | PAP flap [56] | GAP flap [55, 62] |
| Flap type | Myocutaneous flap | Perforator flap | Perforator flap | Myocutaneous flap | Perforator flap | Perforator flap |
| Patient selection criteria | Small breast | Large breast (for salvage) | Large breast | Small to medium breast | Large breast (alternative for DIEP flap) |
| | | Exclusion criteria: desire to have a baby, complicated surgical scars in the abdomen, history of abdominoplasty | | |
| Advantages | Does not require: 1) vascular anastomosis; 2) dissection of perforator | Ease of elevation
Well-concealed scar
Muscle sparing | Large volume so flexibility for breast mound
Abdominoplasty | Muscle sparing
Inconspicuous scar | Large volume
Muscle sparing |
| | | Muscle sparing
Less hernia and bulging [54] (than TRAM flap) | Does not require: 1) vascular anastomosis (pedicled TRAM flap);
2) dissection of perforator | | |
| Disadvantages | Small volume
Volume loss due to muscle atrophy
Intraoperative repositioning
Conspicuous scar | Intraoperative repositioning
Short pedicle [67] | Conspicuous scar | Small volume | Short pedicle [70] |
| | | Requires: 1) vascular anastomosis; 2) dissection of perforator | Volume loss due to muscle atrophy
Hernia and bulging | Requires: 1) vascular anastomosis; 2) dissection of perforator | Intraoperative repositioning
Requires: 1) vascular anastomosis; 2) dissection of perforator |