| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://www.wjon.org |
Original Article
Volume 13, Number 2, April 2022, pages 59-68
The Relationship Between Parametrial Involvement and Parametrial Tissue Removed in Radical Surgery in Early-Stage Cervical Cancer
Ozer Birgea, b, Mehmet Sait Bakira, Selen Dogana, Hasan Aykut Tuncera, Tayup Simseka
aDivision of Gynecologic Oncology, Department of Gynecology Obstetrics, Akdeniz University, Antalya, Turkey
bCorresponding Author: Ozer Birge, Division of Gynecologic Oncology, Department of Gynecology Obstetrics, Akdeniz University, Antalya, Turkey
Manuscript submitted December 11, 2021, accepted March 28, 2022, published online April 23, 2022
Short title: Early-Stage Cervical Cancer
doi: https://doi.org/10.14740/wjon1439
| Abstract | ▴Top |
Background: The study aims to evaluate the effect of parametrial dimensions on the prognosis of cases who underwent type 3 radical hysterectomy or radical trachelectomy in early-stage cervical cancer (stage I - IIa).
Methods: Medical reports of patients with early-stage cervical cancer who have undergone surgery between 1998 and 2020 in Akdeniz University Faculty of Medicine Gynecological Oncology Clinic were reviewed retrospectively. A total of 292 cases were identified and included in the study. Demographic characteristics, preoperative examination findings, operation records, and pathology results of the cases were reviewed.
Results: Parametrial involvement was found histopathologically negative in 244 out of 292 patients included in our study, the remaining 48 (16.4%) patients were found to be positive. The mean length of the right and left parametrium in the group with negative parametrium invasion, who had an average follow-up of 131.2 (0.57 - 268.2) months, was 3 cm, while the mean volume of the right and left parametrium was 7.2 (0.52 - 32) cm3 and 6 (0.48 - 34) cm3, respectively. On the other hand, the mean length of the right and left parametrium was 3 (1.5 - 5.5) cm and 3 (1.4 - 7) cm, respectively, while the mean volume of the right parametrium was 5.55 (1.37 - 22) cm3, and the mean volume of the left parametrium was 7.5 (1.35 - 24) cm3 in 48 patients with positive parametrial invasion. No statistically significant difference was detected between the two groups when compared in terms of parametrial sizes and volumes (P values of 0.061, 0.262, 0.391, and 0.468, respectively).
Conclusions: Radical surgical approach is necessary to obtain a tumor-free surgical margin in the surgical treatment of early cervical cancer, but the complications leading to morbidity and mortality are also increasing with this radicality. For this reason, we consider that it is important to adapt the dimensions of the removed parametrium according to the factors affecting recurrence in cervical cancer to obtain more appropriate surgical margins with the least complications.
Keywords: Early-stage cervical cancer; Parametrial dimensions; Radical hysterectomy; Recurrence; Total survival
| Introduction | ▴Top |
Cervical cancer is the second most common cancer with the highest mortality rate, following breast cancer among women worldwide, and patients with advanced stages have a poor prognosis [1-3]. The incidence of cervical uteri cancer differs in distinct geographical regions of the world. It is the most common gynecological cancer all over the world; however, it is the third most common gynecological cancer following endometrial and ovarian cancer in developed countries [4, 5]. This situation reveals that cervical cancer is a more critical problem in developing countries. The lifetime risk and the incidence are reported as 1.1% and 4/100,000 women, respectively [4]. The most critical risk factor is human papillomavirus (HPV) infection. HPV positivity was detected in 99% of invasive cancer cases [6]. Other risk factors include smoking, multiparity, other sexually transmitted infections, immunosuppression, low socioeconomic level, and multi partnership [7].
Type III radical hysterectomy and pelvic/para-aortic lymphadenectomy are the standard care in early-stage cervical cancer (stage I - IIa). However, the risk of recurrence is up to 30% in patients who receive only surgical treatment [5-7]. Parametria intended to be resected in early-stage cervical malignancy are rich in terms of vascular and nerve fibers; and the operation time, requirement for blood transfusion, and postoperative complications of adjacent organs such as bladder and bowel, may increase especially during radical surgery performed to achieve wide tumor-free surgical margins including parametrium. Furthermore, poor obstetric outcomes have been reported even after radical trachelectomy in young patients scheduled for fertility-sparing surgery [8].
When the studies in the literature are reviewed, parametrial invasion (PI) in cervical cancer is not detected at high rates. It is detected between 5.4% and 30.6% in stage Ib1 early-stage cervical cancer and its incidence varies between 0% and 4.5% in tumors less than 2 cm [9, 10]. Therefore, less radical surgical operations such as conization, simple hysterectomy, and simple trachelectomy are preferred instead of parametrectomy in cases with cervical tumors of stage Ib1 and downstage, especially less than 2 cm, because of their better oncological results [11, 12].
The staging of cervical cancer depends on preoperative imaging together with gynecological examination and assessment of pathology reports after recent radical surgery. Especially in early-stage cervical cancers, disease-free survival (DFS) and overall survival (OS) vary depending on the status of lymph node, parametrium, surgical margin, lymphovascular space invasion (LVSI), cervical stromal invasion, histological type, grade, and tumor size; and the prognosis is poorly affected due to these parameters [12-14]. The patients without these risk factors are defined as a low-risk group. The risk of PI in these cases is below 2% [9, 10]. Therefore, it should be aimed to analyze the length × width × depth measurements of the extracted parametrial dimensions and reveal the effect of the obtained volumetric surgical specimen below specific dimensions on recurrence to reduce morbidity and mortality by avoiding radical surgeries.
In this study, we aim to re-evaluate the pathology reports of patients who have undergone surgery for early-stage cervical cancer and try to reveal the epidemiological features and oncological survival effects depending on the three-dimensional measurements of the parametrium for the first time due to the lack of publications on this subject in the literature.
| Materials and Methods | ▴Top |
The medical records of 292 patients with early-stage (stage I - IIa) cervical tumors operated in Akdeniz University Gynecological Oncology Clinic between 1998 and 2020 were retrospectively analyzed following receiving approval from Akdeniz University Ethics Committee with the decision number KAEK-924 dated September 12, 2020. The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration. Following reviewing the medical records of our patients, 244 (83,6%) cases without parametrium involvement and 48 (16,4%) cases with parametrium involvement were detected. Therefore, our study was designed according to the results of these two groups. Written informed consent of all cases was obtained for both study and publication.
The patients were staged according to the International Federation of Gynecology and Obstetrics (FIGO) 2018 staging system following reviewing the clinical examination, radiological imaging, and pathology reports. Cases with tumors below 4 cm up to stage Ia2 and IIb and without parametrial involvement are included in the study. Patients at stage Ia1, receiving neoadjuvant chemotherapy, undergoing fertility-sparing surgery, with parametrium involvement at stage IIb and above, with second primary cancer, and who refuse treatment were excluded. In the cases up to stage IIb, whose parametrium was clinically and radiologically tumor-free and lymph node involvement negative, patients were then reclassified according to FIGO 2018 staging system depending on the postoperative histopathological results, and these patients were included in the study [4].
Age at diagnosis, gravida, parity, body mass index, preoperative cancer antigen 125 (CA-125) level, initial complaint, HPV status, education level, contraceptive use, smoking status, histopathological diagnosis, tumor dimensions in the pathology report, presence of cervical stromal invasion, presence of lymphovascular stromal invasion, parametrial dimensions in two-dimensional (cm2) and three-dimensional volume (cm3), pelvic and para-aortic lymph node status, tumor stage, type of surgery, surgical margin status, adjuvant therapy, follow-up protocol, recurrence, DFS, OS were recorded.
Pelvic examination, transvaginal ultrasonography (USG), tumor markers, cervical smear, cervical and endocervical biopsies, and pelvic magnetic resonance (MR) imaging were used in the preoperative period. Surgical treatment was modified depending on the extent of the tumor and frozen consultation results. Radical hysterectomy and bilateral pelvic and para-aortic lymphadenectomy (BPPLND) were performed in all cases. In addition, biopsies were obtained in case of suspicion of malignancy during exploration and macroscopic tumoral growths were resected. The surgical specimens were examined by the members of the Pathology Department of our hospital who are experienced in gynecological oncology.
The cases were staged according to the latest FIGO 2018 system [4]. Patients were called for follow-up visits every 3 months in the first postoperative year, and every 6 months for the next 5 years. A comprehensive physical examination, gynecological examination, pelvic/transvaginal USG, serum CA-125 level, and hemogram were performed at each visit. Computed tomography (CT), chest X-ray, and laboratory tests were requested every year. Relapses detected during the follow-up period were determined by imaging methods and pathological examinations in patients considered necessary.
Mean, standard deviation, median, min - max values, and frequencies were used for descriptive statistics by evaluating whether there was a normal distribution or not. Categorical data were expressed as numbers and percentages (%). Parametric methods were used in the analysis of normally distributed variables, and nonparametric methods were used in the analysis of non-normally distributed variables. The dependent t-test was used in the pairwise comparison of independent groups from parametric methods. Mann-Whitney U test was used for pairwise comparison of independent groups from nonparametric methods. Pearson Chi-square, continuity, and Fisher’s exact tests were used to compare categorical data. DFS and OS were calculated by the Kaplan-Meier method, and both groups were compared using log-rank analysis. Statistical Package for the Social Sciences (SPSS) 26 program was used to analyze the data. It was considered statistically significant when the P values in all tests were less than 0.05.
| Results | ▴Top |
Parametrial involvement was found histopathologically negative in 244 out of 292 patients included in our study, the remaining 48 (16.4%) patients were found to be positive. The mean age of the parametrium negative group was 49.9 ± 11.1 years and 54.6 ± 12.8 in the parametrium-positive group; there was a statistically significant difference between the two groups (P = 0.010). There was no significant difference between the two groups regarding gravida, parity, body mass index, and CA-125 levels. The results of both groups were similar in terms of cigarette smoking, which is a risk factor for cervical cancer, and no statistical difference was found (P = 0.775). Postcoital bleeding (38.5% and 33.3%, respectively) was the most common initial complaint in both groups. HPV was found positive in 22 (9%) patients in the parametrium-negative group, six (12.5%) cases with positive HPV test were detected in the parametrium-positive group and this was not statistically significant (P = 0.630). The majority of our patient population did not use contraception. The intrauterine device (IUD) was the most common contraceptive method in the parametrium-negative group. In contrast, oral contraceptive (OC) drug was the most common contraceptive method in the parametrium-positive group, and there was no statistical significance in terms of contraception for the two groups (P = 0.447). When the two groups were compared in terms of education level, a statistically significant difference was found in the parametrium-negative group indicating higher education level due to earlier admission to hospital (P = 0.002). squamous cell tumor was the most frequently detected tumor in both groups (68% and 70.8%, respectively), and there was no statistically significant difference between the two groups in terms of histopathologic types (P = 0.846). Neuroendocrine carcinoma, clear cell carcinoma, and carcinosarcoma were detected in five, two, and one cases, respectively. The most common stage was Ib2 (38.5%) in the parametrium-negative group and Ib3 (25%) in the parametrium-positive group. More cases in the advanced stages were found especially in the parametrium-positive group compared to the negative group. Surgery and adjuvant chemoradiotherapy were the most frequently applied treatment regimen in the parametrium-negative group (102 patients (41.8%)). In comparison, surgery and adjuvant chemoradiotherapy were used in 38 patients (79.2%) in the parametrium-positive group, and there was a statistically significant difference between the two groups (P = 0.001) (Table 1).
 Click to view | Table 1. Clinical and Histopathological Risk Factors of Patients |
The mean length of the right and left parametrium in the group with negative parametrium invasion, who had an average follow-up of 131.2 (0.57 - 268.2) months, was 3 cm, while the mean volume of the right and left parametrium was 7.2 (0.52 - 32) cm3 and 6 (0.48 - 34) cm3, respectively. On the other hand, the mean length of the right and left parametrium was 3 (1.5 - 5.5) cm and 3 (1.4 - 7) cm, respectively, while the mean volume of the right parametrium was 5.55 (1.37 - 22) cm3, and the mean volume of the left parametrium was 7.5 (1.35 - 24) cm3 in 48 patients with positive PI. Considering both dimensions and volume of the parametrium removed by surgery, no statistically significant difference was found between the two groups (P values of 0.061, 0.262, 0.391, and 0.468, respectively) (Table 2).
 Click to view | Table 2. Histopathologic Features and Survival Results of the Patientsa |
The mean diameter of the cervical tumor reported histopathologically was 2.05 (0.5 - 3) cm in the parametrium-negative group, and it was 2.2 (0.6 - 4.6) cm in the parametrium-positive group, and there was no statistically significant difference between the two groups (P = 0.074). However, in subgroup analysis (tumor size < 2 cm and > 2 cm), it was found that the parametrial involvement was positive in 40 patients (19.7%), which was higher in the group with a mass greater than 2 cm. There was a statistically significant difference between the two groups (P = 0.023) (Table 2).
We found a statistically significant difference between the two groups in terms of pathological prognostic risk factors including LVSI, deep stromal invasion (DSI), surgical margin, and lymph node involvement (P values of 0.009, 0.0001, 0.0001, and 0.0001, respectively). Recurrence was detected in 68 (27.9%) patients in the parametrium-negative group and 32 (66.6%) patients in the parametrium-positive group. Forty (16.4%) patients died in the parametrium-negative group, whereas 28 (58.3%) patients died in the parametrium-positive group. There was a statistically significant difference between the two groups regarding recurrence and death (P values of 0.0001 and 0.0001) (Table 2).
Median follow-up for DFS was 131.2 (0.57 - 268.2) months. Five-year DFS was 77.4% in the parametrial-negative group and 44.9% in the parametrium-positive group (Fig. 1). The 5-year OS was 90.2% in the parametrium-negative group, and 66.2% in the parametrium-positive group (Fig. 2).
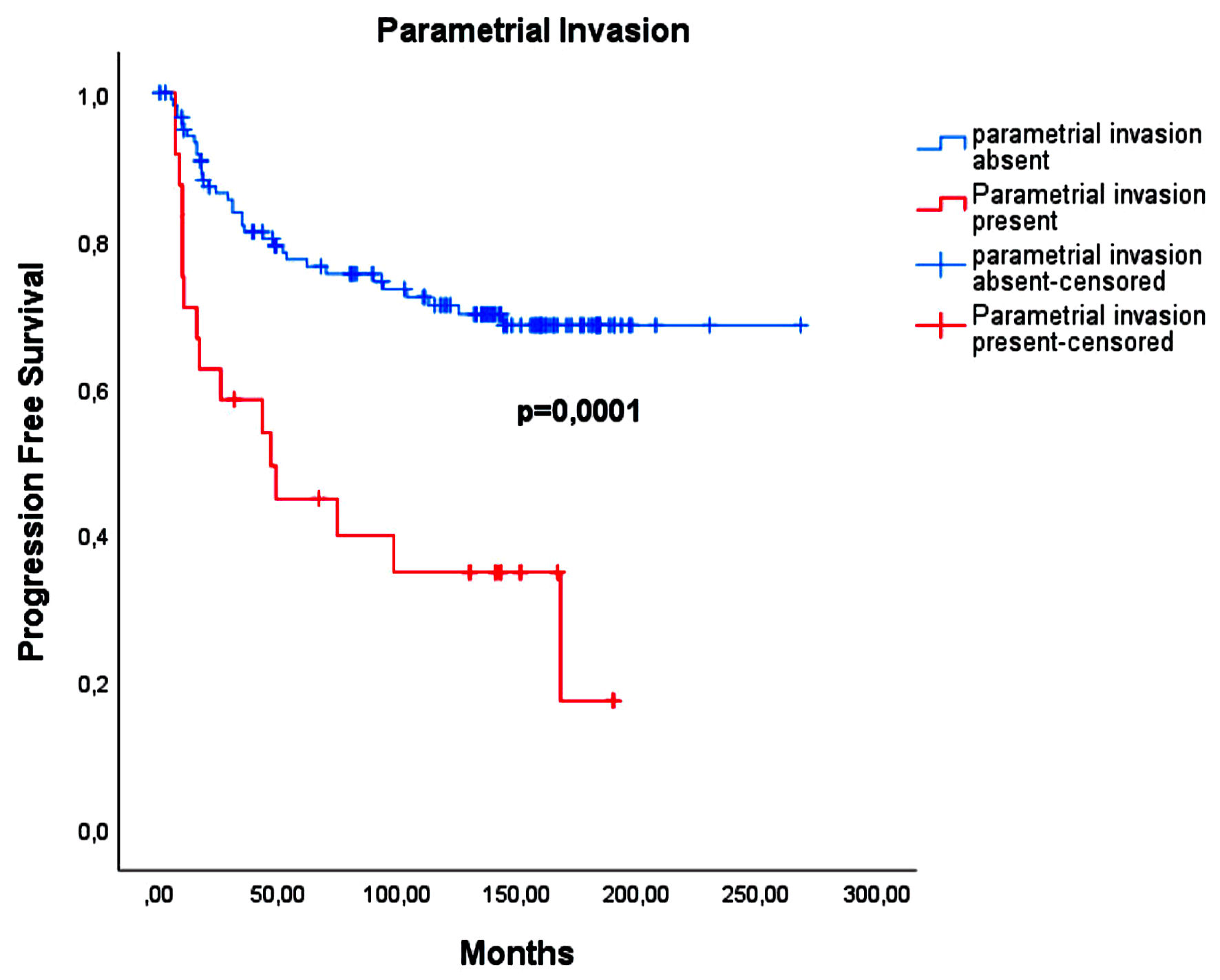 Click for large image | Figure 1. The relationship between disease-free survival and parametrial involvement. |
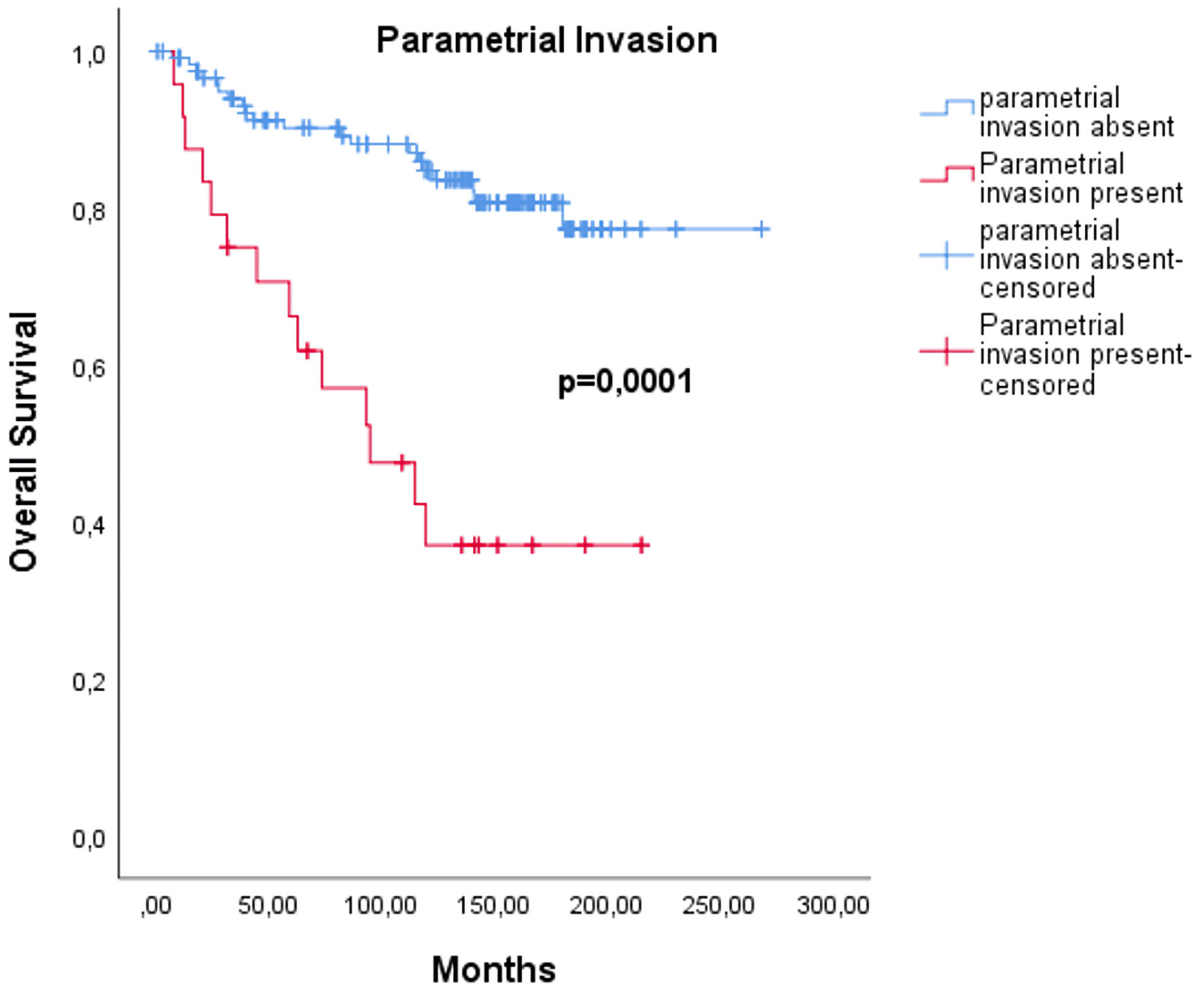 Click for large image | Figure 2. The relationship between overall survival and parametrial involvement. |
| Discussion | ▴Top |
Cervical cancer invades locally through the lymphatic channels and parametrial tissues to the pelvic sidewall. Therefore, the standard treatment approach is en bloc radical surgery, which includes resection of the parametrium with negative surgical margins and the lymphatic system. It is obvious in the literature that, especially the hypogastric nerve is damaged due to resection of parametrium during such a radical extensive surgery, so colorectal disorders, urinary problems may occur, and sexual life can be adversely and permanently affected [15]. In addition, considering the risk factors affecting parametrial involvement, it has been revealed that age is an essential factor in predicting PI, especially in early-stage cervical cancer, and parametrial involvement rates are higher in cervical cancer, especially in elderly patients [16]. However, there have been reports stating the parametrial involvement rates are more common especially in elderly patients due to the shrinkage of the uterus and cervix due to menopausal atrophy, and the easy invasion of the cervical tumor to the paracervical ring by gaining the comparative advantage. It is claimed that the possibility of PI due to atrophic cervix uteri is higher since cervical uteri cancer spreads similarly at all ages [16, 17]. In our study, it is found that the mean age was higher in the parametrial-positive group, and this was statistically significant (P = 0.010) when compared with the parametrial-negative group.
At the end of two- and three-dimensional volumetric examination of the parametrium, which is the general aim of our study, it is clear that there is no dimensional difference between the parametrium-negative and positive groups; therefore, it is very clear that the surgeries are performed in a single center by a team experienced in the field of gynecological oncology. Moreover, the volumetric measurements of the right and left parametrial dimensions indicates that we may not have a significant difference in terms of parametrial involvement; so that the same results can be obtained with less radical surgeries, and thus the complications caused by the removal of wider parametrial tissue in radical surgeries may be avoided.
Early-stage cervical cancer is currently increasing in importance due to its rising incidence. These patients are treated with radical hysterectomy together with pelvic and para-aortic lymphadenectomy in general. The disease is staged using the FIGO system [4]. However, very various prognoses are observed even in patients at the same stage. Therefore, it is essential to determine the prognostic factors affecting the survival rate in these cases. The most critical factor determining the prognosis of cervical cancer is the stage of the disease. As the stage of the disease increases, the response to treatment decreases. Five-year survival in stage I cervical cancer is approximately 80%, and 10% in stage IV cancer [4, 5]. Moreover, As the stage of the disease increases, the possibility of regional lymphatic metastasis increases. This affects the prognosis of cervical cancer negatively. Ten percent of pelvic and 5% para-aortic nodal spread is detected in stage Ib tumors, whereas 30-35% pelvic and 21% para-aortic nodal spread is seen in stage IIb tumors, respectively [18].
The DFS and OS following radical hysterectomy and pelvic and para-aortic lymphadenectomy for cervical cancer vary depending on the status of lymph nodes, tumor size, parametrial involvement, DSI, surgical margin positivity and lymphovascular stromal invasion [5, 13, 19]. Surgical treatment of early-stage invasive cervical cancer consists of radical hysterectomy and pelvic and para-aortic lymph node dissection. Radical hysterectomy involves the removal of the parametrium and one-third or one-half of the upper part of the vagina. Resection of parametrial tissues is essential in the treatment. Because the most common invasion of cervical cancer is through direct microscopic extension to this region or tumor embolism from the primary lesion to the lymph nodes in parametrial tissues. The incidence of parametrial involvement in histopathological examinations ranges between 6% and 31% [19-21]. In our study, the rate of patients with parametrial involvement was 16.4% (48) in a total of 292 patients with early-stage cervical cancer over 22 years, which is compatible with the reviewed literature. Removal of the parametrium during radical hysterectomy is the most common cause of complications. Bladder dysfunction, sexual dysfunction, and anorectal mobility occur due to partial impairment of perfusion as a result of both autonomic nerve damage and disruption of vascular anatomy. Nerve-sparing radical surgery and reduced radicality have recently been introduced in patients with low risk of parametrial involvement, tumor size below 2 cm, LVSI negative, under 50 years of age, below 10 mm DSI, or stage Ib1 superficial invasion [16, 22, 23] to reduce the complications. In our study, when we analyzed the effect of parametrial dimensions on both two-dimensional and three-dimensional parametrial involvement, no statistically significant difference was found; indicating that longer or larger tissue resection does not affect recurrence and survival. It may be recommended to prefer less radical surgical methods in low-risk groups with negative LVSI, under 50 years of age, with normal cervix sizes, and without DSI. Chemoradiotherapy is recommended in most guidelines, especially in cases with advanced-stage cervix cancer with parametrial involvement, and some publications describe the surgical technique of laterally extended parametrectomy. Despite the difficulties, 2% mortality, and up to 70% morbidity rate of this technique, there are case-based and prospective studies describing it at experienced centers to obtain a negative surgical margin laterally. However, the difficulty in the ligation of large vessels (internal iliac artery and vein), anatomical variations in the pelvic sidewall vessels, fibrosis, and technical difficulty in the dissection of previously radio-chemotherapy applied field should be kept in mind [24, 25]. There have been publications declaring that laterally extended parametrectomy is an appropriate technique to surgically obtain a free margin to eliminate pelvic sidewall recurrences [24].
The hypogastric nerve injury has been reported to a lesser extent after a more conservative surgical operation performed for early-stage cervical uteri cancer in the previous studies. Thus, the morbidity rates are lower [26-30]. Moreover, recurrence rate is 4.5%, and the disease-related mortality is 1.25% [31] in the reported studies. Type 1 and type 3 hysterectomy were compared in a prospective study including 125 patients at stage Ib1 to IIa with tumor sizes ranging from 2 to 4 cm, the recurrence rate after type 1 and type 3 hysterectomy was 24% and 13%, respectively after a follow-up time of 280 months, no statistically significant difference was stated between two groups. Furthermore, 73% of the relapsed patients in the type 1 group and 75% of the patients in the type 3 group survived free of disease specific signs after salvage treatment [29]. Morbidities related to blood loss, urinary and bowel dysfunction were determined to be significantly lower in the type 1 hysterectomy group [29, 32].
The incidence of PI in cases with positive lymph node metastasis varies between 36.4% and 48%, so the lymph node metastasis is accepted as one of the most critical risk factors predicting PI [32, 33]. The incidence of parametrial involvement was reported 28% in the early-staged patients with positive sentinel lymph nodes [34]. In our study, the risk of PI is 16.6% (8/48) in early-staged patients with tumors of 2 cm or less. However, removal of the parametrium following the evaluation of lymph node metastasis before hysterectomy in early-stage cervical uteri cancer surgery is still a matter of debate [25, 35].
In recent years, the benefit of parametrial resection in women with early-stage cervical cancer has been questioned. It has been reported that less than 1% of women with early-stage disease and favorable pathological features (tumor < 2 cm, depth of invasion < 10 mm, and negative pelvic nodes) have parametrial involvement [36]. In the ConCerv study, which was the first comprehensive prospective study in 2021, it was also revealed that in early-stage low-risk patients, after conservative surgeries consisting of cervical conization and simple hysterectomy, no tumor was detected at the surgical margin in the hysterectomy material, and oncological results were equivalent to radical surgery [36]. It has been stated that the results obtained so far in the SHAPE and GOG 278 studies, which are two ongoing studies, are also in favor of the conservative surgical approach [37, 38]. In all ConCerv, SHAPE and GOG 278 studies, it is stated that bladder, bowel, and sexual functions and even quality of life are better with less bleeding, fistula, lymphedema and lymphocyst rates.
The current standard treatment for women with early-stage cervical cancer is a radical hysterectomy with removal of the uterus, cervix, upper vagina, and parametrium, as well as pelvic lymph nodes. Conization, with equivalent oncologic results, is an acceptable alternative to radical trachelectomy in women who wish to preserve fertility. This consists of removing the cervix, upper vagina, and parametrium while preserving the uterine fundus, allowing future pregnancy. Although radical hysterectomy and radical trachelectomy result in excellent local tumor control, they can be associated with significant morbidity due to the removal of the parameter involving autonomic nerve fibers associated with bladder, bowel, and sexual function. These radical procedures are also associated with surgical complications such as bleeding, bladder and ureter injury, and fistula formation. Additionally, these procedures require a provider with specialized training in gynecologic oncology surgery, which is not available in most low- and middle-income countries. That is why, considering that more than 85% of cervical cancer is seen in low and moderately developed countries, conization, trachelectomy and simple hysterectomy operations, which are more conservative surgeries, can be applied more easily, especially in cases of early-stage low-risk cervical uteri cancer, and thus, less radical surgery can be performed. Complications are also less common [36, 37, 39-45].
The limitations of our study are being in retrospective nature and possessing varying follow-up time. However, less radical surgical methods can be performed in optimal patients to reduce morbidity and mortality in the near future, particularly as a result of ongoing prospective studies, the HPV vaccine, and the benefits of effective cervical cytological screening methods.
The superiority of our research is that it is carried out in a single center and by a team experienced in long-term gynecological oncology.
In conclusion the radical surgical approach is necessary to obtain a tumor-free surgical margin in the treatment of early cervical cancer, but complications leading to morbidity and mortality increase during parametrial resection. There has been a recent preference of more conservative surgeries in early-stage cervical cancer. For this purpose, we can say that it is important to adapt the size of the extracted parametrium according to the factors affecting recurrence in cervical cancer in order to obtain more suitable surgical margins with the least complication rate.
Acknowledgments
We appreciate the support of the Akdeniz University Hospital.
Financial Disclosure
There was no specific funding source to be mentioned.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Written informed consent of all cases was obtained for both study and publication.
Author Contributions
OB has designed and performed the study. OB, MSB and TS have drafted the manuscript and did critical editing. OB, SD, and HAT have assisted and supported in sample collection and subsequent analysis with statistics. OB and MSB have carefully supervised this manuscript preparation and writing.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Monk BJ, Tewari KS, Koh WJ. Multimodality therapy for locally advanced cervical carcinoma: state of the art and future directions. J Clin Oncol. 2007;25(20):2952-2965.
doi pubmed - Dreyer G. Operative management of cervical cancer. Best Pract Res Clin Obstet Gynaecol. 2005;19(4):563-576.
doi pubmed - Kesic V. Management of cervical cancer. Eur J Surg Oncol. 2006;32(8):832-837.
doi pubmed - Globocan 2018. http://gco.iarc.fr/today/data/factsheets/cancers/23-Cervix-uteri-fact-sheet.pdf.
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7-34.
doi pubmed - Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, Snijders PJ, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189(1):12-19.
doi - International Collaboration of Epidemiological Studies of Cervical Cancer. Comparison of risk factors for invasive squamous cell carcinoma and adenocarcinoma of the cervix: collaborative reanalysis of individual data on 8,097 women with squamous cell carcinoma and 1,374 women with adenocarcinoma from 12 epidemiological studies. Int J Cancer. 2007;120(4):885-891.
doi pubmed - Green TH, Jr., Meigs JV, Ulfelder H, Curtin RR. Urologic complications of radical Wertheim hysterectomy: incidence, etiology, management, and prevention. Obstet Gynecol. 1962;20:293-312.
- Kodama J, Fukushima C, Kusumoto T, Nakamura K, Seki N, Hongo A, Hiramatsu Y. Stage IB1 cervical cancer patients with an MRI-measured tumor size < or = 2 cm might be candidates for less-radical surgery. Eur J Gynaecol Oncol. 2013;34(1):39-41.
- Gemer O, Eitan R, Gdalevich M, Mamanov A, Piura B, Rabinovich A, Levavi H, et al. Can parametrectomy be avoided in early cervical cancer? An algorithm for the identification of patients at low risk for parametrial involvement. Eur J Surg Oncol. 2013;39(1):76-80.
doi pubmed - Biliatis I, Kucukmetin A, Patel A, Ratnavelu N, Cross P, Chattopadhyay S, Galaal K, et al. Small volume stage 1B1 cervical cancer: Is radical surgery still necessary? Gynecol Oncol. 2012;126(1):73-77.
doi pubmed - Bouchard-Fortier G, Reade CJ, Covens A. Non-radical surgery for small early-stage cervical cancer. Is it time? Gynecol Oncol. 2014;132(3):624-627.
doi pubmed - Sedlis A, Bundy BN, Rotman MZ, Lentz SS, Muderspach LI, Zaino RJ. A randomized trial of pelvic radiation therapy versus no further therapy in selected patients with stage IB carcinoma of the cervix after radical hysterectomy and pelvic lymphadenectomy: A Gynecologic Oncology Group Study. Gynecol Oncol. 1999;73(2):177-183.
doi pubmed - Morice P, Piovesan P, Rey A, Atallah D, Haie-Meder C, Pautier P, Sideris L, et al. Prognostic value of lymphovascular space invasion determined with hematoxylin-eosin staining in early stage cervical carcinoma: results of a multivariate analysis. Ann Oncol. 2003;14(10):1511-1517.
doi pubmed - Rob L, Halaska M, Robova H. Nerve-sparing and individually tailored surgery for cervical cancer. Lancet Oncol. 2010;11(3):292-301.
doi - Kodama J, Kusumoto T, Nakamura K, Seki N, Hongo A, Hiramatsu Y. Factors associated with parametrial involvement in stage IB1 cervical cancer and identification of patients suitable for less radical surgery. Gynecol Oncol. 2011;122(3):491-494.
doi pubmed - Merz E, Miric-Tesanic D, Bahlmann F, Weber G, Wellek S. Sonographic size of uterus and ovaries in pre- and postmenopausal women. Ultrasound Obstet Gynecol. 1996;7(1):38-42.
doi pubmed - Heller PB, Maletano JH, Bundy BN, Barnhill DR, Okagaki T. Clinical-pathologic study of stage IIB, III, and IVA carcinoma of the cervix: extended diagnostic evaluation for paraaortic node metastasis—a Gynecologic Oncology Group study. Gynecol Oncol. 1990;38(3):425-430.
doi - Delgado G, Bundy B, Zaino R, Sevin BU, Creasman WT, Major F. Prospective surgical-pathological study of disease-free interval in patients with stage IB squamous cell carcinoma of the cervix: a Gynecologic Oncology Group study. Gynecol Oncol. 1990;38(3):352-357.
doi - Covens A, Rosen B, Murphy J, Laframboise S, DePetrillo AD, Lickrish G, Colgan T, et al. How important is removal of the parametrium at surgery for carcinoma of the cervix? Gynecol Oncol. 2002;84(1):145-149.
doi pubmed - Benedetti-Panici P, Maneschi F, D'Andrea G, Cutillo G, Rabitti C, Congiu M, Coronetta F, et al. Early cervical carcinoma: the natural history of lymph node involvement redefined on the basis of thorough parametrectomy and giant section study. Cancer. 2000;88(10):2267-2274.
doi - Roh JW, Lee DO, Suh DH, Lim MC, Seo SS, Chung J, Lee S, et al. Efficacy and oncologic safety of nerve-sparing radical hysterectomy for cervical cancer: a randomized controlled trial. J Gynecol Oncol. 2015;26(2):90-99.
doi pubmed - Kim MK, Kim JW, Kim MA, Kim HS, Chung HH, Park NH, Park IA, et al. Feasibility of less radical surgery for superficially invasive carcinoma of the cervix. Gynecol Oncol. 2010;119(2):187-191.
doi pubmed - Capilna ME, Ungar L, Cozlea AL, Gheorghe M, Stanca M, Lintner B, Moldovan AA. Laterally extended parametrectomy. Obstet Gynecol Sci. 2021;64(5):470-472.
doi pubmed - Marnitz S, Tsunoda AT, Martus P, Vieira M, Affonso Junior RJ, Nunes J, Budach V, et al. Surgical versus clinical staging prior to primary chemoradiation in patients with cervical cancer FIGO stages IIB-IVA: oncologic results of a prospective randomized international multicenter (Uterus-11) intergroup study. Int J Gynecol Cancer. 2020;30(12):1855-1861.
doi pubmed - Bisseling KC, Bekkers RL, Rome RM, Quinn MA. Treatment of microinvasive adenocarcinoma of the uterine cervix: a retrospective study and review of the literature. Gynecol Oncol. 2007;107(3):424-430.
doi pubmed - Fagotti A, Gagliardi ML, Moruzzi C, Carone V, Scambia G, Fanfani F. Excisional cone as fertility-sparing treatment in early-stage cervical cancer. Fertil Steril. 2011;95(3):1109-1112.
doi pubmed - Kasamatsu T, Okada S, Tsuda H, Shiromizu K, Yamada T, Tsunematsu R, Ohmi K. Early invasive adenocarcinoma of the uterine cervix: criteria for nonradical surgical treatment. Gynecol Oncol. 2002;85(2):327-332.
doi pubmed - Landoni F, Maneo A, Zapardiel I, Zanagnolo V, Mangioni C. Class I versus class III radical hysterectomy in stage IB1-IIA cervical cancer. A prospective randomized study. Eur J Surg Oncol. 2012;38(3):203-209.
doi pubmed - Naik R, Cross P, Nayar A, Mayadevi S, Lopes A, Godfrey K, Hatem H. Conservative surgical management of small-volume stage IB1 cervical cancer. BJOG. 2007;114(8):958-963.
doi pubmed - Reade CJ, Eiriksson LR, Covens A. Surgery for early stage cervical cancer: how radical should it be? Gynecol Oncol. 2013;131(1):222-230.
doi pubmed - Puente R, Guzman S, Israel E, Poblete MT. Do the pelvic lymph nodes predict the parametrial status in cervical cancer stages IB-IIA? Int J Gynecol Cancer. 2004;14(5):832-840.
doi pubmed - Wright JD, Grigsby PW, Brooks R, Powell MA, Gibb RK, Gao F, Rader JS, et al. Utility of parametrectomy for early stage cervical cancer treated with radical hysterectomy. Cancer. 2007;110(6):1281-1286.
doi pubmed - Strnad P, Robova H, Skapa P, Pluta M, Hrehorcak M, Halaska M, Rob L. A prospective study of sentinel lymph node status and parametrial involvement in patients with small tumour volume cervical cancer. Gynecol Oncol. 2008;109(2):280-284.
doi pubmed - Hsu HC, Tai YJ, Chen YL, Chiang YC, Chen CA, Cheng WF. Factors predicting parametrial invasion in patients with early-stage cervical carcinomas. PLoS One. 2018;13(10):e0204950.
doi pubmed - Schmeler KM, Pareja R, Lopez Blanco A, Humberto Fregnani J, Lopes A, Perrotta M, Tsunoda AT, et al. ConCerv: a prospective trial of conservative surgery for low-risk early-stage cervical cancer. Int J Gynecol Cancer. 2021;31(10):1317-1325.
doi pubmed - Plante M. The SHAPE trial. http://www.gcig.igcs.org/Spring2012/2012_june_shape_trial.pdf.
- Covens A. GOG Protocol 278. http://www.gcig.igcs.org/Spring2012/2012_june_cervix_cancer_committee.pdf.
- Piver MS, Rutledge F, Smith JP. Five classes of extended hysterectomy for women with cervical cancer. Obstet Gynecol. 1974;44(2):265-272.
- Low JA, Mauger GM, Carmichael JA. The effect of Wertheim hysterectomy upon bladder and urethral function. Am J Obstet Gynecol. 1981;139(7):826-834.
doi - Kadar N, Saliba N, Nelson JH. The frequency, causes and prevention of severe urinary dysfunction after radical hysterectomy. Br J Obstet Gynaecol. 1983;90(9):858-863.
doi pubmed - Sood AK, Nygaard I, Shahin MS, Sorosky JI, Lutgendorf SK, Rao SS. Anorectal dysfunction after surgical treatment for cervical cancer. J Am Coll Surg. 2002;195(4):513-519.
doi - Rosenquist A, Bergman K, Strang P. Optimizing hospital-based home care for dying cancer patients: a population-based study. Palliat Med. 1999;13(5):393-397.
doi pubmed - Bodurka DC, Sun CC, Frumovitz MM. Quality of life in cervix cancer survivors—what matters the most in the long-term? Gynecol Oncol. 2005;97(2):307-309.
doi pubmed - Wu J, Logue T, Kaplan SJ, Melamed A, Tergas AI, Khoury-Collado F, Hou JY, et al. Less radical surgery for early-stage cervical cancer: a systematic review. Am J Obstet Gynecol. 2021;224(4):348-358.e345.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Oncology is published by Elmer Press Inc.


