| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://www.wjon.org |
Case Report
Volume 13, Number 4, August 2022, pages 235-240
Syringomatous Tumor of the Nipple
Nicole M. Favrea, Quratulain Sabihb, Joseph C. L’Huilliera, b, Kazuaki Takabea, b, c, d, e, f, Helen Cappuccinob, g
aDepartment of Surgery, University at Buffalo, Jacobs School of Medicine and Biomedical Sciences the State University of New York, Buffalo, NY 14203, USA
bDepartment of Surgical Oncology, Roswell Park Comprehensive Cancer Center, Buffalo, NY 14263, USA
cDepartments of Gastroenterological Surgery, Yokohama, Kanagawa 236-004, Japan
dDepartment of Breast Surgery and Oncology, Tokyo Medical University, Tokyo 160-8402, Japan
eDepartment of Surgery, Niigata University Graduate School of Medical and Dental Sciences, Niigata 951-8510, Japan
fDepartment of Breast Surgery, Fukushima Medical University, Fukushima 960-1247, Japan
gCorresponding Author: Helen Cappuccino, Department of Surgical Oncology, Roswell Park Comprehensive Cancer Center, Buffalo, NY 14263, USA
Manuscript submitted June 29, 2022, accepted August 1, 2022, published online August 23, 2022
Short title: Syringomatous Tumor of the Nipple
doi: https://doi.org/10.14740/wjon1513
| Abstract | ▴Top |
Syringomatous tumor of the nipple (SyT), previously known as syringomatous adenoma of the nipple (SAN) was originally described in 1983 as a rare benign tumor of the sweat duct. It is a rare benign tumor arising from the skin adnexal eccrine glands that can be misdiagnosed as invasive carcinoma due to its infiltrative nature, resulting in overtreatment. We report clinical, histopathologic, and surgical findings of a case of infiltrating syringomatous adenoma in a 40-year-old female as well as a literature review of previous cases. A high index of suspicion is required to make the diagnosis of SyT and prevent overtreatment.
Keywords: Syringomatous tumor of the nipple; Infiltrating syringomatous adenoma; Nipple; Benign breast lesions; Breast neoplasm
| Introduction | ▴Top |
Syringomatous adenoma of the nipple (SAN) was originally described in 1983 as a rare benign tumor of the sweat duct [1]. In 1989, the qualifier “infiltrating” was added to portray its potentially locally infiltrative nature, although the same paper also noted its inability to metastasize [2]. This entity is now known as “syringomatous tumor of the nipple (SyT)” as described in the most recent edition of the World Health Organization (WHO) classification of breast neoplasms [3]. It is postulated to arise from sweat glands, given the distinct histologic appearance resembling sweat ducts within the nipple-areolar complex. SyT can be misdiagnosed as invasive carcinoma due to its infiltrative nature, resulting in overtreatment.
We present a case of SyT in a 40-year-old female and include a review of literature. The main purpose of reviewing this entity is to review its clinical presentation, histological presentation and to discuss treatment recommendations.
| Case Report | ▴Top |
A 40-year-old female with multinodular goiter, irritable bowel syndrome, and anxiety presented with a 2-year history of painful right nipple enlargement. One year prior to presenting to us, the patient had a benign breast biopsy for an unrelated cyst in the right breast lower inner quadrant. Symptoms included sharp pain that would “bring the patient to her knees” but there were no other breast complaints (nipple discharge, skin changes, or palpable breast masses).
On examination, the right nipple was notably larger, denser, and more turgid feeling (Fig. 1). It could also not be reduced manually or with warm compresses. There were no signs of ulceration, additional skin changes, or breast masses.
 Click for large image | Figure 1. A 40-year-old woman with 2-year history of pain and right nipple enlargement. (a) Macroscopic findings of the nipples. Note the deformity and enlargement of the right nipple compared to the normal left nipple. |
Mammography and targeted ultrasound were unremarkable (Fig. 2a, b). Breast magnetic resonance imaging (MRI) showed asymmetric enhancement of the right nipple (Fig. 3). Nipple excision vs. fine needle aspiration vs. incisional nipple biopsy were reviewed with the patient. After almost 2 years of watchful waiting and expectant management patient with ongoing complaints of nipple pain, she elected for excisional biopsy of her right nipple. Preoperatively, she met with plastic surgery to discuss delayed reconstruction.
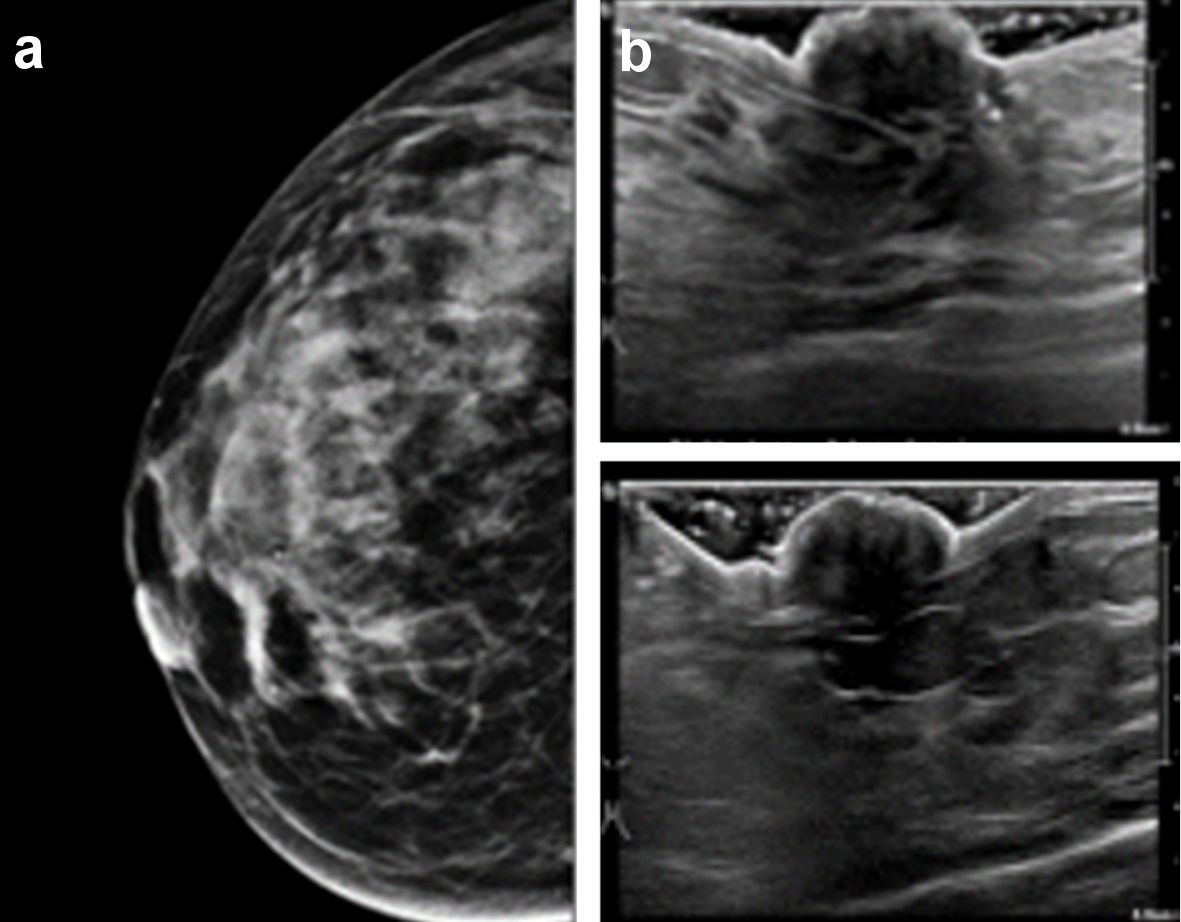 Click for large image | Figure 2. (a) Mammography of the right breast. No retro-areolar calcifications nor abnormalities were seen on regular or magnified views. (b) Ultrasonography of the right nipple. No retro-areolar masses or abnormalities were seen. |
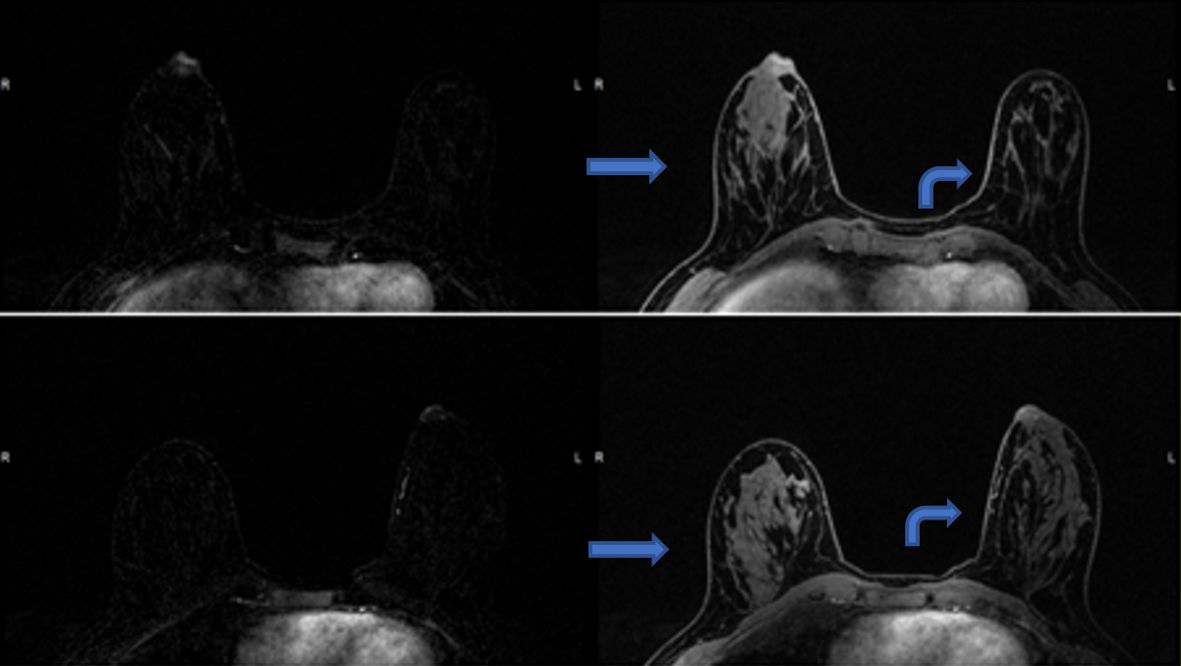 Click for large image | Figure 3. Post-contrast T1-weighted fat-suppressed axial MRI images, with subtractions on the left, show asymmetric enhancement of the right nipple (arrows) compared to the left (curved arrows). MRI: magnetic resonance imaging. |
Histopathology revealed an infiltrative epithelial tumor growing through the dermis, infiltrating through bundles of areolar smooth muscle with focal perineural invasion (Fig. 4a-d). Superficially, the tumor contained dilated keratinaceous cysts that transitioned into squamous nests. Deeper in the specimen, the tumor formed ductal structures, some having a syringoid appearance and many showing compressed lumens. Cytologically, these cells were bland and contained only one to two mitoses per 10 high-power fields. The ducts had a retained peripheral myoepithelial layer that was stained by p40 and smooth muscle actin (SMA). There was no evidence of carcinoma in situ. Retention of the myoepithelial layer, superficial location, and lack of atypia distinguish syringomatous tumor from adenosquamous carcinoma. This pathology is like microcystic adnexal carcinoma of the skin, another rare entity, a low-grade sweat gland carcinoma that is typically seen in the head and neck region.
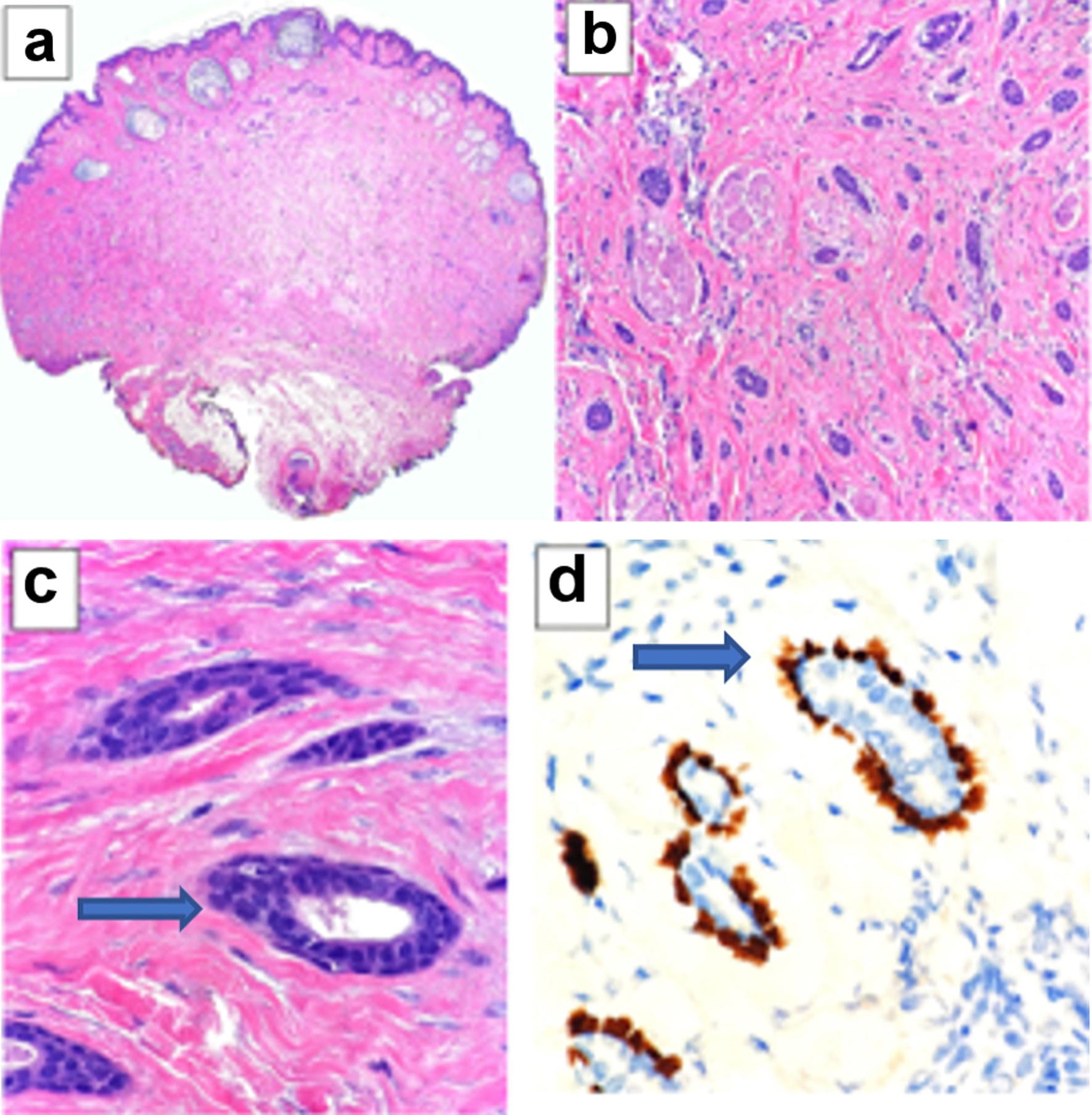 Click for large image | Figure 4. (a) At low power, superficial keratin-filled cysts are seen (H&E stain, × 20). Deeper in the dermis is an infiltrative proliferation of small epithelial clusters and cords that extend down to the adipose tissue below. This configuration is similar to microcystic adnexal carcinoma, a sweat gland tumor usually seen on skin of the head and neck. (b) Many of the cellular clusters have a syringoid ductal appearance. They are seen infiltrating around and through bundles of dermal smooth muscle (H&E stain, × 200). (c) At high power the ducts have a uniform and cytologically bland cuboidal luminal layer (arrow), and a peripheral outer layer of flattened basal cells is frequently identified (H&E stain, × 600). (d) P40 immunohistochemical stain. The intact basal cell layer (arrow) is highlighted by p40 immunohistochemical stain (× 600). H&E: hematoxylin and eosin. |
| Discussion | ▴Top |
SyT is a rare entity, with presentation, clinical and radiographic findings difficult to distinguish from malignancy. Histological examination is needed to differentiate SyT from other similar entities, including duct ectasia, tubular and nipple adenoma, ductal carcinoma in situ, Paget’s disease of the nipple, intraductal papilloma, and low-grade adenosquamous carcinoma. For example, nipple adenomas are an entity described by Leo et al as benign neoplasms of major lactiferous duct epithelium; however, malignancy can be found elsewhere in the breast [4]. Here, we have identified 17 cases described in the literature since 2004 after the comprehensive review of the topic by Carter et al (Table 1) [5-21].
 Click to view | Table 1. Seventeen Cases of SAN Reported in the Literature Since 2004 |
Of those 17 cases, there were 16 in women and a single case in a male, which was the second male case reported in the literature [6]. Patients varied in age from 23 to 71 years old, with a median age of 40. Most cases were localized to a single breast, but there were two reports of synchronous bilateral SyTs [7, 9] and one report of SyT in a supernumerary nipple [9].
The clinical presentation of SyT varies widely. The most common clinical presentation was a firm, enlarged nipple/areolar, or sub/peri nipple/areolar mass, with/without nipple inversion, which may or may not be painful/tender, and persistent nipple erection. Two patients had reported nipple discharge, one patient was diagnosed post-partum [5, 9]. Similarly, our patient presented with unilateral nipple enlargement, erection, and associated pain. Mass size on initial presentation varied from 0.5 to 7 cm, although larger size was not associated with worse outcome.
Mammogram findings ranged from normal, to nonspecific, to variably sized calcifications or asymmetry at the nipple-areolar complex or subareolar region. Ultrasound often confirmed the mammographic findings and noted irregularly outlined nodules in the subareolar region of the nipple. One study reported an irregular mass with enhancement on contrast computed tomography (CT), suspicious for malignancy [10]. Only one report noted MRI findings, an irregular mass in the subareolar region of the nipple [11]. Our patient’s breast MRI, related to the symptomatic nipple, noted asymmetric enhancement of the right nipple. This review reveals that imaging of SyT cannot distinguish it from other neoplasms and cannot be trusted to distinguish SyT from carcinoma of the breast.
Histologically, SyT is identical to a syringoma, a benign tumor that arises in the dermal sweat gland ducts; therefore, clinical characteristics are needed to differentiate the two entities. As SyTs are diagnosed based on histopathologic characteristics, all of the reported cases in the literature revealed similar findings. Classically, the histologic characteristics include two cell layers resembling a teardrop, with disorganized cordlike tubules and ducts. A clear layer of myoepithelial cells between the epithelial cells and fibrous stroma is often visible [12]. Two main immunohistochemical markers that stain positive in SyT are p63 and SMA.
It is imperative to distinguish SyT from malignant entities. Deformity of the nipple, with increased turgidity, and persistent erection of the nipple are common with SyT. It can present with or without pain, in the case presented, perineural invasion likely explains the pain. It does not generally involve disruption in the integrity of the epidermis (which helps to distinguish it from Paget’s disease). A lack of associated inflammation helps to rule out infectious or inflammatory diagnoses. Superficial breast malignancy would be the most likely diagnosis with which SyT could be confused. Nipple adenoma and large duct papilloma are also included in differential diagnosis. Nipple adenomas are usually identified by their lack of stromal tissue, and intra-ductal papilloma most commonly present with nipple discharge, both pathognomonic features to help differentiate them from SyT.
Regarding treatment, wide local excision to clear margins is recommended. Given the paucity of cases, it is hard to know the exact extent of excision necessary. With recurrences being rare, a conservative approach to excisions is suggested. Neither metastasis nor subsequent cases of breast cancer have been reported in these patients.
Conclusions
SyT can present a challenging clinical diagnosis, which is often made only after excision. Recurrence is only a concern if SyT is not excised to negative margins; there are no known associations with other breast pathologies and no specific demographic showing increased prevalence. Awareness of this rare benign tumor is crucial to avoid overtreatment with mastectomy, aggressive local excisions, or lymph node biopsies. Given the rarity of SyT, no specific guidelines exist for its treatment; till date, simple wide local excision to clear margins is indicated with no assessment of the lymph nodes needed.
Learning points
SyT is a rare, benign tumor with the appearance of sweat ducts.
Due to its infiltrative nature, SyT can be misdiagnosed as invasive carcinoma, resulting in overtreatment.
We present a case in which prolonged breast pain is the presenting symptom of SyT.
Awareness of this rare tumor is crucial to avoid overtreatment.
Acknowledgments
We thank Dr. Cindy Wong (Department of Radiology, Roswell Park Comprehensive Cancer Center, Elm and Carlton Streets, Buffalo, NY 14263, USA), and Dr. Paul Bogner (Department of Pathology, Roswell Park Comprehensive Cancer Center, Elm and Carlton Streets, Buffalo, NY 14263, USA) for their help.
Financial Disclosure
This research was supported by National Institutes of Health, USA Grant Number R37CA248018, R01CA250412, R01CA251545, R01EB029596, as well as US Department of Defense BCRP Grant number W81XWH-19-1-0674 and W81XWH-19-1-0111 to K.T. National Cancer Institute; Cancer Center Support Grant P30CA016056 supports Roswell Park Comprehensive Cancer Center.
Conflict of Interest
The authors have no conflict of interest to declare.
Informed Consent
Informed consent was obtained from the patient for publication of the details of her case.
Author Contributions
The study was designed by authors NF, QS, JL, KT, and HC. Literature search was conducted by authors NF and QS. Data collection was performed by authors NF, QS, and JL. Data analysis was performed by authors NF, QS, JL, KT, and HC. Data interpretation was performed by authors NF, QS, KT, and HC. The paper was written by authors NF, QS, and JL with critical revisions provided by KT and HC.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Rosen PP. Syringomatous adenoma of the nipple. Am J Surg Pathol. 1983;7(8):739-745.
doi pubmed - Jones MW, Norris HJ, Snyder RC. Infiltrating syringomatous adenoma of the nipple. A clinical and pathological study of 11 cases. Am J Surg Pathol. 1989;13(3):197-201.
doi pubmed - Rakha E, Reis-Filho J, Sasano H, Wu Y. Neuroendocrine neoplasms: introduction (5th edn), WHO classification of tumours, vol. 2. IARC Press, Lyon. 2019.
- Leo ME, Carter GJ, Waheed U, Berg WA. Nipple adenoma: correlation of imaging findings and histopathology. J Breast Imaging. 2022;4(4):408-412.
doi pubmed - Carter E, Dyess DL. Infiltrating syringomatous adenoma of the nipple: a case report and 20-year retrospective review. Breast J. 2004;10(5):443-447.
doi pubmed - Paramaguru R, Ramkumar S. Syringomatous adenoma of the nipple in a male breast: a case report with a brief review of literature and histomorphological approach to diagnosis. Cureus. 2021;13(11):e19586.
doi pubmed - Montgomery ND, Bianchi GD, Klauber-Demore N, Budwit DA. Bilateral syringomatous adenomas of the nipple: Case report with immunohistochemical characterization of a rare tumor mimicking malignancy. Am J Clin Pathol. 2014;141(5):727-731.
doi pubmed - Mrklic I, Bezic J, Pogorelic Z, Ilic N, Tadic T, Buljevic V, Tomic S. Synchronous bilateral infiltrating syringomatous adenoma of the breast. Scott Med J. 2012;57(2):121.
doi pubmed - Page RN, Dittrich L, King R, Boulos F, Page DL. Syringomatous adenoma of the nipple occurring within a supernumerary breast: a case report. J Cutan Pathol. 2009;36(11):1206-1209.
doi pubmed - Zhong MH, Zhu HL, Zheng WT, Han JD. Infiltrating syringomatous adenoma of the nipple: a case report. J Am Acad Dermatol. 2013;69(4):e190-191.
doi pubmed - Ishikawa S, Sako H, Masuda K, Tanaka T, Akioka K, Yamamoto Y, Hosokawa Y, et al. Syringomatous adenoma of the nipple: a case report. J Med Case Rep. 2015;9:256.
doi pubmed - Abeciunas V, Jurgaitis K, Jakutis N. Recurrent syringomatous adenoma of the nipple following a misdiagnosis: A case report. Niger J Clin Pract. 2020;23(9):1324-1327.
doi pubmed - Yosepovich A, Perelman M, Ayalon S, Papa M, Kopolovic J. Syringomatous adenoma of the nipple: a case report. Pathol Res Pract. 2005;201(5):405-407.
doi pubmed - Oliva VL, Little JV, Carlson GW. Syringomatous adenoma of the nipple—treatment by central mound resection and oncoplastic reconstruction. Breast J. 2008;14(1):102-105.
doi pubmed - Riaz N, Khan SM, Idrees R, Kayani N. Infiltrating syringomatous adenoma of nipple. J Coll Physicians Surg Pak. 2008;18(7):438-439.
- Sarma DP, Stevens T. Infiltrating syringomatous eccrine adenoma of the nipple: a case report. Cases J. 2009;2:9118.
doi pubmed - Odashiro M, Lima MG, Miiji LN, Odashiro DN, Carvalho GV, Prates Campos JC, Odashiro AN. Infiltrating syringomatous adenoma of the nipple. Breast J. 2009;15(4):414-416.
doi pubmed - Kim HM, Park BW, Han SH, Moon HJ, Kwak JY, Kim MJ, Kim EK. Infiltrating syringomatous adenoma presenting as microcalcification in the nipple on screening mammogram: case report and review of the literature of radiologic features. Clin Imaging. 2010;34(6):462-465.
doi pubmed - AlSharif S, Tremblay F, Omeroglu A, Altinel G, Sun S, Mesurolle B. Infiltrating syringomatous adenoma of the nipple: Sonographic and mammographic features with pathologic correlation. J Clin Ultrasound. 2014;42(7):427-429.
doi pubmed - Zhu M, Jia BS, Peng YL. [Multiple calcification of the nipple areola complex: a case report of infiltrating syringomatous adenoma of the nipple]. Sichuan Da Xue Xue Bao Yi Xue Ban. 2020;51(6):878-880.
- Niakan S, Patino A, Jadhav N, Hadro J, Crisi GM, Mason H. Syringomatous adenoma of the nipple with microcalcifications on mammography: A case report. Breast J. 2021;27(2):170-172.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Oncology is published by Elmer Press Inc.


