| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://www.wjon.org |
Case Report
Volume 14, Number 2, April 2023, pages 158-163
Esophageal Perforation in a 76-Year-Old Man After C5-C7 Anterior Discectomy and Anterior Plate Fusion
Lexi Frankela, Amalia D. Ardeljanb, Gabriela Santizob, Maximiliano Guerrab, Ghargi Gharatb, Sarmed Alnajarb, Divesh Manjanib, Andrew Ardeljanb, Kazuaki Takabec, d, Omar M. Rashida, b, e, f, g, h, i, j, k
aNova Southeastern University, Dr. Kiran C. Patel College of Allopathic Medicine, Fort Lauderdale, FL, USA
bDepartment of Surgery, Michael and Dianne Biennes Comprehensive Cancer Center, Holy Cross Health, Fort Lauderdale, FL, USA
cDepartment of Surgical Oncology, Roswell Park Comprehensive Cancer Center, Buffalo, NY, USA
dDepartment of Surgery, University at Buffalo Jacobs School of Medicine and Biomedical Sciences, the State University of New York, Buffalo, NY, USA
eUniversity of Miami, Leonard Miami School of Medicine, Miami, FL, USA
fDepartment of Surgical Oncology, Massachusetts General Hospital, Boston, MA, USA
gDepartment of Surgical Oncology, Broward Health, Fort Lauderdale, FL, USA
hTopLine MD Alliance, Fort Lauderdale, FL, USA
iDepartment of Surgical Oncology Memorial Health, Pembroke Pines, FL, USA
jDepartment of Surgical Oncology, Delray Medical Center, Delray, FL, USA
kCorresponding Author: Omar M. Rashid, Complex General Surgical Oncology, General & Robotic Surgery, TopLine MD Alliance, Fort Lauderdale, FL 33308, USA
Manuscript submitted December 29, 2022, accepted March 6, 2023, published online March 24, 2023
Short title: Esophageal Perforation After ACDF
doi: https://doi.org/10.14740/wjon1563
| Abstract | ▴Top |
Anterior cervical discectomy and fusion (ACDF) is indicated for the treatment of various cervical pathologies, including myelopathy, cervical disc degeneration, and radiculopathy. Esophageal perforation is a rare postsurgical complication of ACDF, although it poses serious and potentially fatal outcomes. Esophageal perforation has been described as the most fatal complication of the gastrointestinal tract as delayed diagnosis can lead to sepsis and death. Diagnosis of this complication is often difficult because it can be masked by various symptoms such as recurrent aspiration pneumonia, fever, dysphagia, and neck pain. While this complication usually occurs within the first 24 h post-surgery, it can also develop later and persist chronically in rare cases. Awareness and early recognition of this complication may improve outcomes and reduce mortality and morbidity. A 76-year-old man underwent C5-C7 ACDF in October 2017. A thorough review of the patient’s postoperative condition included computed tomography (CT) and esophagogram, which were negative for signs of acute complications. The postoperative recovery was uneventful until several months post-procedure when he began to develop vague dysphagia and weight loss of unknown etiology. A CT scan was obtained 6 months postoperatively and was negative for perforation. He then underwent a battery of inconclusive procedures and scans at multiple institutions. After several months of persistent dysphagia and weight loss without a diagnosis, the patient presented to our network for further workup and treatment recommendations. Upper endoscopy was performed and showed fistulization between the esophagus and the metal hardware in the cervical spine. Esophagram demonstrated no obstruction but decreased peristalsis of the lower esophagus and lateral rightward deviation of the left upper cervical esophagus with minimal mucosal irregularities. These findings were secondary to mass effect of the cervical plate. The patient was successfully treated with a surgical approach using esophagogastroduodenoscopy (EGD) guided repair in layers and a sternocleidomastoid muscle flap. This report demonstrates a rare case of delayed esophageal perforation after ACDF and successful treatment of the perforation by surgical repair using the dual technique.
Keywords: Anterior cervical fusion; Anterior discectomy; Dysphagia; Esophagography; Postoperative complications
| Introduction | ▴Top |
Anterior cervical discectomy and fusion (ACDF) is indicated for the treatment of various cervical pathologies, including myelopathy, cervical disc degeneration, and radiculopathy [1, 2]. Esophageal perforation is a rare post-surgical complication of ACDF, although it poses serious and potentially fatal outcomes [3]. Esophageal perforation has been described as the most fatal complication of the gastrointestinal tract as delayed diagnosis can lead to sepsis and death [1]. Diagnosis of this complication is often difficult because it can be masked by various symptoms such as recurrent aspiration pneumonia, fever, dysphagia, and neck pain. While this complication usually occurs within the first 24 h post-surgery, it can also develop later and persist chronically in rare cases. Perforations that occur in the delayed setting often cause more extensive damage, making prevention and early detection essential to decrease long-term complications and morbidity [1]. Awareness and appropriate management are therefore crucial for outcome improvement.
In this case report, we describe a 76-year-old man who presented with a history of C5-C7 ACDF due to cervical stenosis associated with left upper extremity pain and weakness. Early postoperative recovery was uneventful and the patient did not experience signs of esophageal perforation, including dysphagia and unintentional weight loss, until several months later in the delayed period. This report describes the serious impact of delayed esophageal perforation following ACDF and the impact of its early recognition on outcomes and survival.
| Case Report | ▴Top |
Investigations
A 76-year-old man underwent C5-C7 ACDF in October 2017. Postoperative follow-up and examination included CT and esophagogram, which were negative for signs of acute complications. The postoperative recovery was uneventful and the patient denied any persistent neurological symptoms or symptoms of infection. At 6 months post-procedure, he developed vague dysphagia and weight loss of unknown etiology. A CT of cervical spine was obtained 6 months postoperatively and was negative for perforation (Fig. 1). X-rays of the cervical spine on flexion and extension at 6 months showed appropriate placement of the anterior plate and screws at C5, C6, and C7 with no motion across the fused levels. CT of the neck at 6 months postoperatively demonstrated mild residual multilevel foraminal narrowing with appropriate placement of the hardware and satisfactory surgical fusion from C5-C7 with no significant canal stenosis. Nevertheless, the patient reported dysphagia and continued weight loss regardless of the battery of inconclusive procedures and scans he underwent at multiple institutions.
 Click for large image | Figure 1. Computed tomography of cervical spine 6 months postoperatively. Red arrow indicates cervical plate. |
The patient’s past medical history includes hypertension, hyperlipidemia, chronic obstructive pulmonary disease (COPD), gastroesophageal reflux disease (GERD), benign prostatic hyperplasia and history of right nephrectomy approximately 20 years prior to presentation due to renal cancer. Patient denied current or past use of tobacco products or illicit drugs and reported moderate consumption of alcohol. The patient’s father had a history of kidney failure and his mother had a history of heart failure.
Diagnosis
After 6 more months of persistent dysphagia and weight loss without a diagnosis, the patient presented to our network for further workup and treatment recommendations. CT of the neck 12 months postoperatively showed anterior cervical plate in adequate position with air between the plate and esophagus (Fig. 2). An upper endoscopy was performed at 12 months postoperatively, which showed fistulization between the esophagus and the metal hardware in the cervical spine. An esophagram was also performed, which demonstrated no obstruction but decreased peristalsis of the lower esophagus and lateral rightward deviation of the left upper cervical esophagus with minimal mucosal irregularities. Esophagram also showed involvement of the posterior wall of the cervical esophagus overlying the anterior plate and screws without evidence of leak or fistula (Fig. 3).
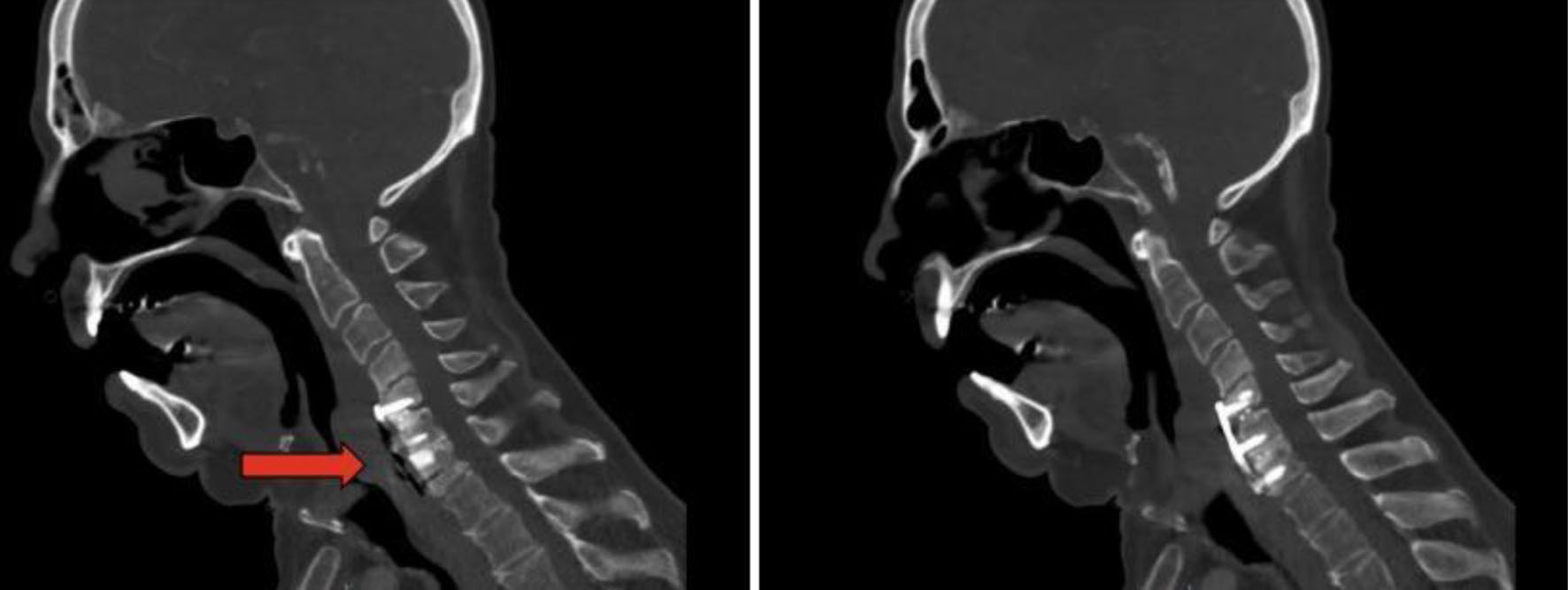 Click for large image | Figure 2. Computed tomography of the neck 12 months postoperatively. Anterior cervical plate in adequate position with air between the plate and esophagus. |
 Click for large image | Figure 3. Esophagram at 12 months. Red arrow indicates defect. The image shows contiguity between the lumen of the esophagus and the cervical hardware based on the transit of the oral contrast, consistent with a posterior esophageal wall perforation contained by the cervical hardware without extravasation. |
Management and treatment
The patient was initially managed with pre-habilitation goals prior to surgery, including feeding tube placement and nutrition optimization in preparation for a staged approach to repair the esophageal defect. After the induction of anesthesia, the patient presented with bradycardia and hypotension, and underwent successful resuscitation. Following stabilization of the patient, a cardiology workup was performed, including nuclear stress testing, and was negative for any abnormalities.
One month later, the patient underwent removal of the cervical spine hardware and a surgical repair guided by EGD (Fig. 4) with muscle flap reinforcement (Fig. 5). A feeding gastrostomy tube was placed and both the procedure and postoperative period were uncomplicated. The patient was discharged 6 days after surgery with a JP drain and gastric tube feedings.
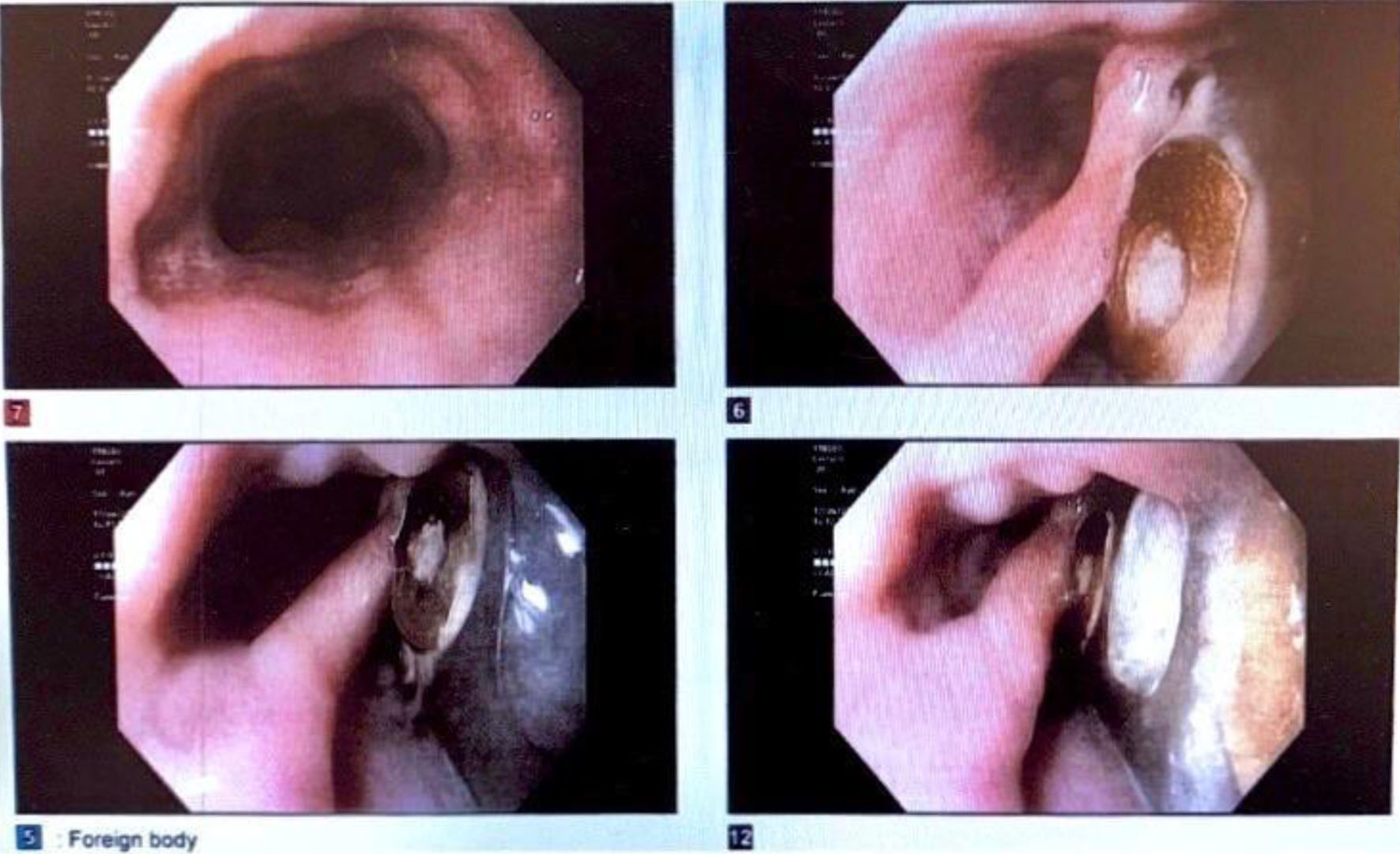 Click for large image | Figure 4. Esophagogastroduodenoscopy 12 months postoperatively. Image displays the cervical hardware, which had eroded through the posterior wall of the cervical esophagus concordant with the esophagram, which had demonstrated contiguity between the lumen of the esophagus and the cervical hardware based on the transit of the oral contrast, consistent with a posterior esophageal wall perforation contained by the cervical hardware without extravasation. These findings were also consistent with the patient’s chronic presentation without sepsis. |
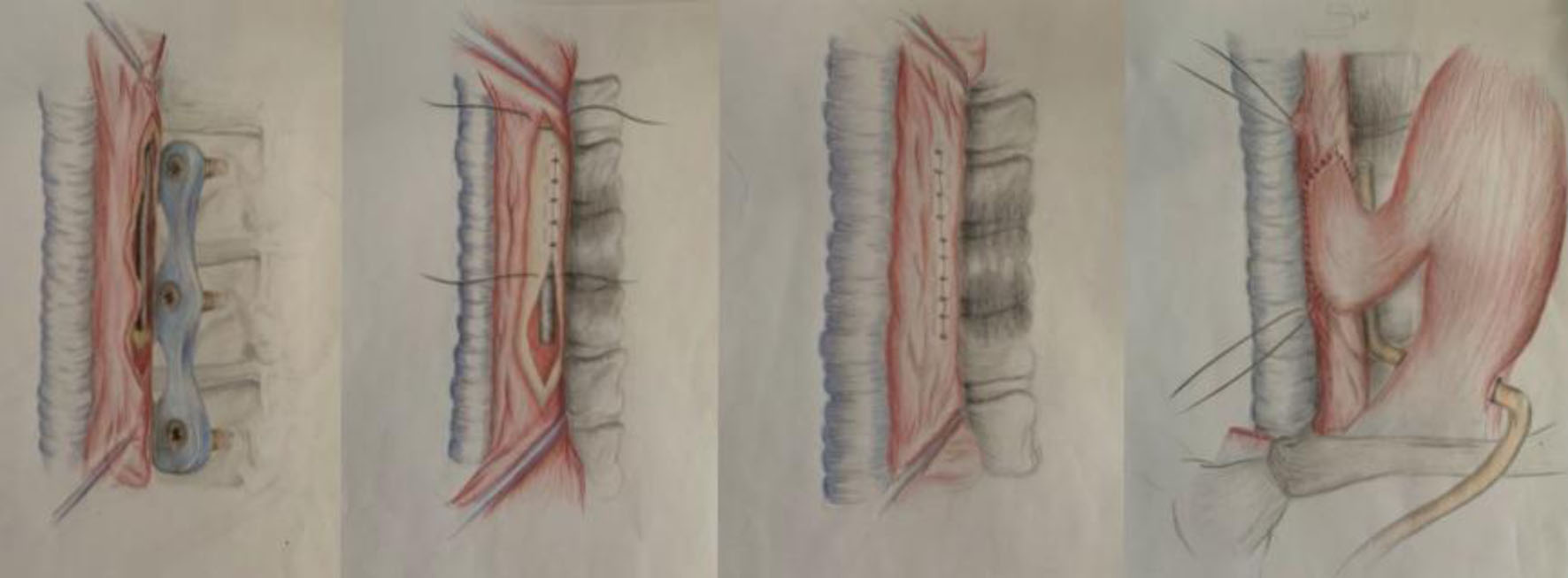 Click for large image | Figure 5. Representation of surgical repair guided by esophagogastroduodenoscopy in layers and muscle flap reinforcement. |
In a follow-up visit, esophagram demonstrated a completely healed operatory wound without evidence of leakage. A modified barium swallow was performed and did not reveal any abnormalities (Fig. 6). The patient continued tolerating liquids with minimal JP output and no evidence of dysphagia, aspiration or infection. The patient performed optimally on speech evaluation without aspiration, his voice returned to baseline, and he progressed back to solid food.
 Click for large image | Figure 6. Postoperative barium swallow demonstrating resolution of obstruction. |
| Discussion | ▴Top |
ACDF has been used since the late 1950s by spinal neurosurgeons and orthopedic surgeons to treat patients with persistent neurological symptoms and pain despite non-surgical methods. The anterior approach to the cervical spine is considered a safe and versatile technique, with positive clinical outcomes and low morbidity and mortality [4-7]. The global complication rate of anterior cervical procedures is 13.2% and is mainly comprised of minor setbacks, necessitating minimal or no further intervention [8]. Significant complications following ACDF include soft tissue swelling and hematoma, recurrent laryngeal nerve injury, carotid artery injury, cerebrospinal fluid leakage, root and cord injury, superficial wound infection and tracheoesophageal injury [4, 5, 9, 10]. While soft tissue injury is a recognized complication of the anterior approach, the incidence of perforation from all causes varies between 0.25% and 1.49% [11] and the global incidence of esophageal perforation fluctuates between 0% and 3.4% [4]. The rarity of this diagnosis and the variability of its incidence reported in previous studies and between different institutions makes esophageal perforation in the setting of ACDF a difficult diagnosis and requires a high index of clinical suspicion.
As the cervical spine sits directly posterior to the esophagus, the esophagus necessitates mobilization for spinal access for ACDF [12]. Perforation during mobilization is rare because several esophageal layers, including adventitia, longitudinal and circular muscle, submusocosal and mucosal layers, all must be damaged before a full puncture can occur [12]. However, there are two areas of esophageal weakness where perforation is most likely, which include Killian’s triangle and the thyrohyoid membrane [12]. Esophageal retraction and esophageal manipulation intraoperatively are the most common causes of perforation, followed by hardware failure [11]. If the perforation is recognized intraoperatively, a simple primary suture repair is needed. However, if the perforation is diagnosed postoperatively, treatment is often more extensive, requires further surgery, and risks serious and life-threatening complications [5, 10].
Esophageal perforation is a serious complication that may occur weeks to months to as late as 8 - 10 years after surgery [10]. Causes of delayed esophageal injury include chronic irritation, compression of the esophagus by the hardware, and chronic friction between the posterior wall of the esophagus and the planting system. In this case, the patient presented with dysphagia and mild weight loss 1 year after ACDF; considering the delayed presentation, this patient’s diagnosis was likely secondary to chronic friction and subsequent perforation. The ability of esophageal perforation to present in the delayed period combined with its variable presentation makes esophageal injury important to consider and treat in the setting of post-surgical dysphagia, fever, swelling, subcutaneous emphysema, or any sign of infection [5].
Basic treatment of delayed esophageal perforation depends on the size of perforation [7]. Antibiotics as monotherapy or other non-surgical treatment options are indicated only if the defect size is less than 1 cm in asymptomatic patients [6]. Surgical treatment is the gold standard if the diameter is greater than 1 cm or the patient has any signs or symptoms of local infection. Surgical intervention includes drainage of any abscesses, removal of hardware and repair of the perforation site [6]. In these instances, primary closure with or without muscle flap interposition should be performed. In this case, the patient presented with dysphagia without signs of infection and esophagoscopy revealed an exposed cervical plate in the esophageal lumen, which qualified for surgical repair [6, 7].
In contrast to esophageal perforation, dysphagia after surgery is very common, with a reported prevalence between 28% and 57% of cases [5, 6]. Nevertheless, most cases follow a transient course resolving spontaneously within 2 years post-surgically. Identifying which patients require a more detailed workup for esophageal perforation is still a challenge for clinicians. As delays in diagnosis and treatment increase morbidity and mortality exponentially, workup should be completed as soon as perforation is suspected, especially in the context of persistent dysphagia [13].
Conclusion
Delayed esophageal perforation post-ACDF has an extremely low incidence and presents variably which makes diagnosis of this complication exceedingly difficult. However, it should always be considered in patients with chronic dysphagia or signs of local infection after ACDF.
In this report, we discussed case of delayed esophageal perforation without instrumental failure occurring 1 year after ACDF. High suspicion, recognition, proper treatment, and long-term follow-up are crucial for improving post-surgical outcomes and decreasing the morbidity and mortality of this life-threating pathology. Decreasing the incidence of esophageal perforation after ACDF may translate into not only improved clinical outcomes, but also a reduction in the hospital length of stay, the readmissions rate, and overall healthcare costs.
Acknowledgments
The authors acknowledge the support of Holy Cross Hospital and Nova Southeastern University Dr. Kiran C. Patel College of Allopathic Medicine.
Financial Disclosure
Grant support by Broward Community Foundation.
Conflict of Interest
None to declare.
Informed Consent
Patient consent for case report was obtained.
Author Contributions
Lexi Frankel is responsible for manuscript writing and literature review. Amalia Ardeljan is responsible for figures and supplemental manuscript editing. Gabriela Santizo, Maximiliano Guerra, Ghargi Gharat, Sarmed Alnajar, Divesh Manjani and Andrew Ardeljan are responsible for manuscript writing and figure editing. Kazuaki Takabe and Omar Rashid are responsible for manuscript writing, editing, and data analysis.
Data Availability
The data supporting the findings of this study have been extracted from PearlDiver national database and available from the corresponding author upon reasonable request.
| References | ▴Top |
- Fengbin Y, Xinwei W, Haisong Y, Yu C, Xiaowei L, Deyu C. Dysphagia after anterior cervical discectomy and fusion: a prospective study comparing two anterior surgical approaches. Eur Spine J. 2013;22(5):1147-1151.
doi - Gaudinez RF, English GM, Gebhard JS, Brugman JL, Donaldson DH, Brown CW. Esophageal perforations after anterior cervical surgery. J Spinal Disord. 2000;13(1):77-84.
doi - Hershman SH, Kunkle WA, Kelly MP, Buchowski JM, Ray WZ, Bumpass DB, Gum JL, et al. Esophageal perforation following anterior cervical spine surgery: case report and review of the literature. Global Spine J. 2017;7(1 Suppl):28S-36S.
doi - Shriver MF, Lewis DJ, Kshettry VR, Rosenbaum BP, Benzel EC, Mroz TE. Dysphagia Rates after Anterior Cervical Diskectomy and Fusion: A Systematic Review and Meta-Analysis. Global Spine J. 2017;7(1):95-103.
doi - Tasiou A, Giannis T, Brotis AG, Siasios I, Georgiadis I, Gatos H, Tsianaka E, et al. Anterior cervical spine surgery-associated complications in a retrospective case-control study. J Spine Surg. 2017;3(3):444-459.
doi - Eroglu A, Turkyilmaz A, Aydin Y, Yekeler E, Karaoglanoglu N. Current management of esophageal perforation: 20 years experience. Dis Esophagus. 2009;22(4):374-380.
doi - Fountas KN, Kapsalaki EZ, Machinis T, Robinson JS. Extrusion of a screw into the gastrointestinal tract after anterior cervical spine plating. J Spinal Disord Tech. 2006;19(3):199-203.
doi - Nathani A, Weber AE, Wahlquist TC, Graziano GP, Park P, Patel RD. Delayed presentation of pharyngeal erosion after anterior cervical discectomy and fusion. Case Rep Orthop. 2015;2015:173687.
doi - Nourbakhsh A, Garges KJ. Esophageal perforation with a locking screw: a case report and review of the literature. Spine (Phila Pa 1976). 2007;32(15):E428-435.
doi - Yang SY, Lee SB, Cho KS. Delayed esophagus perforation after anterior cervical spine surgery. Korean J Neurotrauma. 2015;11(2):191-194.
doi - Newhouse KE, Lindsey RW, Clark CR, Lieponis J, Murphy MJ. Esophageal perforation following anterior cervical spine surgery. Spine (Phila Pa 1976). 1989;14(10):1051-1053.
doi - Yue WM, Brodner W, Highland TR. Persistent swallowing and voice problems after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year follow-up study. Eur Spine J. 2005;14(7):677-682.
doi - Zhong ZM, Jiang JM, Qu DB, Wang J, Li XP, Lu KW, Xu B, et al. Esophageal perforation related to anterior cervical spinal surgery. J Clin Neurosci. 2013;20(10):1402-1405.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Oncology is published by Elmer Press Inc.


