| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://www.wjon.org |
Original Article
Volume 15, Number 1, February 2024, pages 90-99
Multicentricity and the Risk of Recurrence/Persistence After Laser Vaporization for High-Grade Vulvar and Vaginal Intraepithelial Neoplasia
Sathone Boonlikita, c , Punyacha Tangterdchanakita, b
aDepartment of Obstetrics and Gynecology, Rajavithi Hospital, College of Medicine, Rangsit University, Bangkok, Thailand
bDepartment of Obstetrics and Gynecology, Pakkred Hospital, Nonthaburi, Thailand
cCorresponding Author: Sathone Boonlikit, Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Rajavithi Hospital, Rachathewee District, Bangkok 10400, Thailand
Manuscript submitted October 20, 2023, accepted December 13, 2023, published online January 10, 2024
Short title: Laser Vaporization for Multicentric VIN/VAIN
doi: https://doi.org/10.14740/wjon1743
| Abstract | ▴Top |
Background: The aim of the study was to assess the effect of multicentricity on the recurrence/persistence of high-grade vulvar intraepithelial neoplasia (VIN) and vaginal intraepithelial neoplasia (VAIN) after laser vaporization.
Methods: A retrospective cohort study was conducted on patients diagnosed with high-grade VIN/VAIN, who had undergone laser vaporization between 1997 and 2014. Recurrence/persistence rates and factors affecting recurrence/persistence were analyzed, and a life table analysis of recurrence-free intervals was conducted.
Results: Among the 65 patients, the recurrence/persistence rate following laser vaporization was 22.3 per 100 person-years, with a median time to recurrence/persistence of 31.2 months (95% confidence interval (CI): 0.0 - 71.9 months). Patients with multicentricity and unicentricity had a recurrence/persistence rate of 49.1 per 100 person-years, with a median time to recurrence/persistence of 11.4 months, and 7.4 per 100 person-years, with a median time to recurrence/persistence of 96.5 months, respectively (P = 0.0002). The difference in recurrence-free survival between the multicentricity and unicentricity groups was significant (P = 0.00035). Patients with multicentricity had a 4.7-fold higher risk of recurrence/persistence (hazard ratio (HR): 4.71, 95% CI: 1.87 - 11.88, P = 0.001). Multivariate analysis showed that multicentricity was an independent risk factor for recurrence/persistence (odds ratio (OR): 4.16, 95% CI: 1.56 - 11.06, P = 0.004).
Conclusions: Treatment of multicentric, high-grade VIN/VAIN with laser vaporization is strongly associated with treatment failure, with approximately half of patients experiencing recurrence/persistence.
Keywords: Multicentricity; Multicentric disease; Multicentric lower genital tract disease; Multicentric intraepithelial neoplasia; Laser vaporization; Vulvar intraepithelial neoplasia; Vaginal intraepithelial neoplasia
| Introduction | ▴Top |
Carbon dioxide (CO2) laser vaporization is widely accepted as an effective treatment for vulvar intraepithelial neoplasia (VIN) and vaginal intraepithelial neoplasia (VAIN) [1-3]. Unlike those of the more common high-grade cervical intraepithelial neoplasia (CIN), the outcomes of patients with high-grade VIN/VAIN following laser vaporization remain uncertain. Although the risk of recurrence may be higher with laser vaporization vs. excision [4, 5], studies have reported conflicting results [4-12]. A meta-analysis showed that laser vaporization and excision were probably equally effective in patients with high-grade VIN [2]. A small, randomized prospective study of VAIN patients reported no differences in regression rates among the laser vaporization, vaginal imiquimod, and expectant management groups during short-term follow-up [9]. Despite its many advantages, a major concern related to laser vaporization is the high incidence of recurrence [3-5, 7, 11].
Several prognostic factors have been shown to affect recurrence after treatment of VIN/VAIN, such as age, immunosuppression, human papillomavirus (HPV) persistence, smoking, method of treatment, large lesion size, multifocal lesions, and multicentric lesions [3, 4, 6-8, 10-15]. The concept of multicentric lower genital tract disease, defined as intraepithelial lesions or cancer at two or three sites (cervix, vagina, and vulva), is well recognized [1, 7, 13, 16-18]. Multiple primary preinvasive or invasive lesions involving the cervix, vagina, vulva, perianal area, and anus can occur synchronously or metachronously [1, 13, 18]. Multicentricity is a common feature and an important prognostic factor in lower genital tract neoplasia [1, 4, 5, 7, 13, 14]. Patients with VIN/VAIN are likely to have the clinical features of multicentricity, i.e., prior or concurrent intraepithelial neoplasia (IN) or worse (IN+) of the lower genital tract at two or three sites [3, 5-7, 11, 19]. In our institute, many patients with VIN/VAIN have prior or concurrent high-grade IN+ of the lower genital tract, and a high proportion of these patients subsequently experience recurrence/persistence.
We aimed to retrospectively review recurrence/persistence in patients with high-grade VIN/VAIN following CO2 laser vaporization at the Rajavithi Hospital, Bangkok, Thailand, in order to determine whether multicentricity was associated with recurrence/persistence and to identify other risk factors.
| Materials and Methods | ▴Top |
The study was performed in the Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Rajavithi Hospital, Bangkok, Thailand. The protocol for the project received ethical approval from the Institutional Review Board (Ethics Committee of Rajavithi Hospital). This study was conducted in compliance with the ethical standards of our institution on human subjects as well as with the Helsinki Declaration. A retrospective cohort study was performed on women with histologically confirmed high-grade VIN or high-grade VAIN, who were treated with CO2 laser vaporization (including both newly diagnosed patients who had CO2 laser vaporization as a first-line treatment and recurrent cases who had previously undergone failed non-laser therapy) at the Rajavithi Hospital, Bangkok, Thailand, between January 1997 and December 2014. Patients were excluded if they did not have histologically confirmed high-grade VIN/VAIN, had been diagnosed with concurrent invasive carcinoma of the vulva or vagina at initial presentation, or had laser excision alone without documented vaporization. Patients were evaluated by colposcopy, and the diagnosis was established based on histology of biopsies. If patients had multiple histological specimens showing different grades of IN, the highest grade was assigned as the final histological diagnosis.
Demographic and clinical data (recurrence/persistence, progression to cancer, and potential risk factors affecting recurrence) were retrospectively retrieved from medical records. Regarding CO2 laser vaporization, Access CO2® laser equipment (PLC Medical Systems, Milford, USA) was used in Rajavithi Hospital until 2006, followed by Ultra MD® 40 (Laser engineering, Nashville, USA) in 2007 - 2010 and AcuPulse® (Luminis, Dreieich-Dreieichenhain, Germany) since 2011. Colposcopy-guided laser was performed using a Zeiss® colposcope (Carl Zeiss Surgical Gmb H, Oberkochen, Germany) with a micromanipulator at a focal distance of 300 mm. For hairy areas of the vulva, a power of 10 - 15 W and super pulse mode were used. For non-hairy areas of the vulva or vagina, a power of 20 - 25 W and continuous wave mode were used. All lesions were treated by covering all the edge and the normal skin or mucosa ≥ 0.5 cm around the lesions at optimal depth. The optimal depth for VIN treatment depended on the location of lesions; those in non-hairy areas were vaporized to the second surgical plane reaching the superficial papillary dermis or a depth of 1 mm, while lesions in hairy areas were vaporized to the third surgical plane reaching the mid reticular dermis or a depth of 2 - 3 mm. The optimal depth for VAIN treatment was at the lamina propria of the vagina or a depth of 1 - 1.5 mm. The selection for treatment by laser depended on the surgeon’s opinion and intention. Laser was performed by gynecologic oncologists in an operation room, and most procedures were conducted under general anesthesia in an outpatient setting.
After treatment, multiple early follow-up visits were scheduled for wound examination. Thereafter, patients were followed up at 3 - 6-month intervals with vulvovaginal examination. For VIN, visual inspection of the vulva with or without colposcopy was performed. For VAIN, vaginal examination and cytology with or without colposcopy were conducted. HPV testing was not performed during the follow-up period, during which, if any abnormality was found, biopsy of the suspicious lesion was performed. Patients were followed up until completion of the study period, loss to follow-up, or death.
The primary outcomes were recurrence (defined as redevelopment of histology-proven high-grade VIN/VAIN or worse after a period of regression) and persistence (defined as histology-proven high-grade VIN/VAIN or worse at the first follow-up visit after laser); these were analyzed together as a single outcome. Regression (i.e., cure) after laser was defined as the absence of recurrence/persistence. Recurrence-free survival (RFS) was defined as the time interval (in months) between treatment and the occurrence of recurrence and/or persistence or the date of the last clinical follow-up. In the present study, characteristics of multicentric lower genital tract diseases were categorized into two kinds of definition. First, multicentricity was defined as previous or concurrent high-grade IN or worse (high-grade IN+) of the lower genital tract at two or three sites (cervix, vagina, and vulva). Second, the alternative definition of multicentric lower genital tract disease used in the present study was multicentric IN of the lower genital tract (multicentric IN) which included high-grade IN of two or three sites in lower genital tract, excluding invasive lesion; lesions may have arisen at the same time (synchronous lesions) or at separate times (metachronous lesions).
Pearson’s Chi-square test and Fisher’s exact test were used for categorical variables and Student’s t-test for continuous ones. The occurrence of recurrence/persistence onset in a sample per unit of person-time during follow-up was assessed using the incidence rate. Cumulative 6-month and 1-, 2-, and 5-year RFS rates in patients treated with laser vaporization were calculated. Recurrence-free intervals according to both definitions of multicentric lower genital tract disease (multicentricity and multicentric IN) were assessed and compared using the Kaplan-Meier method, log-rank (Mantel-Cox) test and Cox’s proportional hazards model. Risk factors predictive of recurrence/persistence were determined, using the odds ratio approximation for the relative risk ratio, and P values were derived from two-tailed tests. Multivariate analysis was performed using Cox’s proportional hazards model to determine covariates significantly associated with recurrence/persistence, and a P value ≤ 0.05 was considered statistically significant. The data were analyzed using IBM® SPSS® for Windows version 22.0 (IBM Corp., Armonk, NY, USA).
| Results | ▴Top |
Sixty-seven patients were treated with CO2 laser vaporization at Rajavithi Hospital during the study period. Four were excluded: one was lost to follow-up after operation, while histology-proven high-grade VIN/VAIN could not be confirmed in three cases. A total of 63 patients, all of whom were Asian, were included; however, 65 high-grade VIN/VAIN cases were treated with CO2 laser vaporization during the study period because two patients were each diagnosed with both high-grade VIN and high-grade VAIN at different times and underwent laser operations on the vulva and vagina. One patient had the treatments on two separate visits while the other one had both at the same visit. Table 1 shows the patient characteristics. Nineteen (29.2%) had high-grade VIN, and 51 (78.4%) had high-grade VAIN. Five cases had histological diagnosis of both high-grade VIN and high-grade VAIN in each individual, but not all of them (only two) received laser operations at both sites. Multicentricity was present in 38 (58.4%) patients. The two most common associated diseases were CIN2/3 and cervical cancer, which were observed in 19 (29.2%) and 15 (23.0 %) cases, respectively. Most multicentric lesions (32/38) occurred metachronously. Nine (13.8%) patients had a history of pelvic radiation. All patients attended for follow-up, and the median follow-up period was 11.4 months (range: 0.4 - 111.5 months). During follow-up, 36 cases did not have recurrence/persistence, while the remaining 29 did, resulting in a recurrence/persistence rate following laser vaporization of 22.3 per 100 person-years with a median time to recurrence/persistence of 31.2 months (95% confidence interval (CI): 0.0 - 71.9 months). The cumulative 6-month, 1-, 2- and 5-year RFS rates were 80.1%, 65.3%, 52.4%, and 41.6 %, respectively (Table 2). The life table analysis of RFS is displayed in Figure 1. Two patients with an initial diagnosis of high-grade VAIN progressed to invasive vaginal cancer. Patients with multicentricity had a recurrence/persistence rate of 49.1 per 100 person-years with a median time to recurrence/persistence of 11.4 months (95% CI: 5.7 - 17.2 months), while patients with unicentricity had a recurrence/persistence rate of 7.4 per 100 person-years with a median time to recurrence/persistence of 96.5 months (95% CI: 21.0 - 172.1 months) (P = 0.0002). There was a very highly significant difference in RFS between the multicentricity and unicentricity groups (P = 0.00035) (Fig. 2), and laser vaporization in patients with multicentricity was associated with a 4.7-fold higher risk of recurrence/persistence (hazard ratio (HR): 4.71, 95% CI: 1.87 - 11.88, P = 0.001). Table 3 summarizes the risk factors for recurrence/persistence. Univariate analysis revealed that recurrence/persistence was associated with several factors, including previous or concurrent neoplasia of the lower genital tract (odds ratio (OR): 3.84, 95% CI: 1.19 - 12.32, P = 0.02), multicentricity (OR: 5.11, 95% CI: 1.66 - 15.67, P = 0.003), previous or concurrent invasive cancer of the lower genital tract (OR: 5.47, 95% CI: 1.52 - 19.6, P = 0.009), history of pelvic radiation (OR: 13.33, 95% CI: 1.55 - 114.2, P = 0.008), and laser for recurrent cases (OR: 2.56, 95% CI: 1.86 - 3.53, P = 0.006). In the multivariate analysis, multicentricity (OR: 4.16, 95% CI: 1.56 - 11.06, P = 0.004), history of pelvic radiation (OR: 6.33, 95% CI: 2.39 - 16.72, P = 0.000), and laser for recurrent cases (OR: 5.34, 95% CI: 2.00 - 14.22, P = 0.001) were found to be independent risk factors for recurrence/persistence.
 Click to view | Table 1. Patient Characteristics |
 Click to view | Table 2. Recurrence-Free Survival (RFS) Rates in Patients Treated With Laser Vaporization |
 Click for large image | Figure 1. Kaplan-Meier life table analysis of recurrence-free survival in high-grade VIN/VAIN patients following laser vaporization. VIN: vulvar intraepithelial neoplasia; VAIN: vaginal intraepithelial neoplasia. |
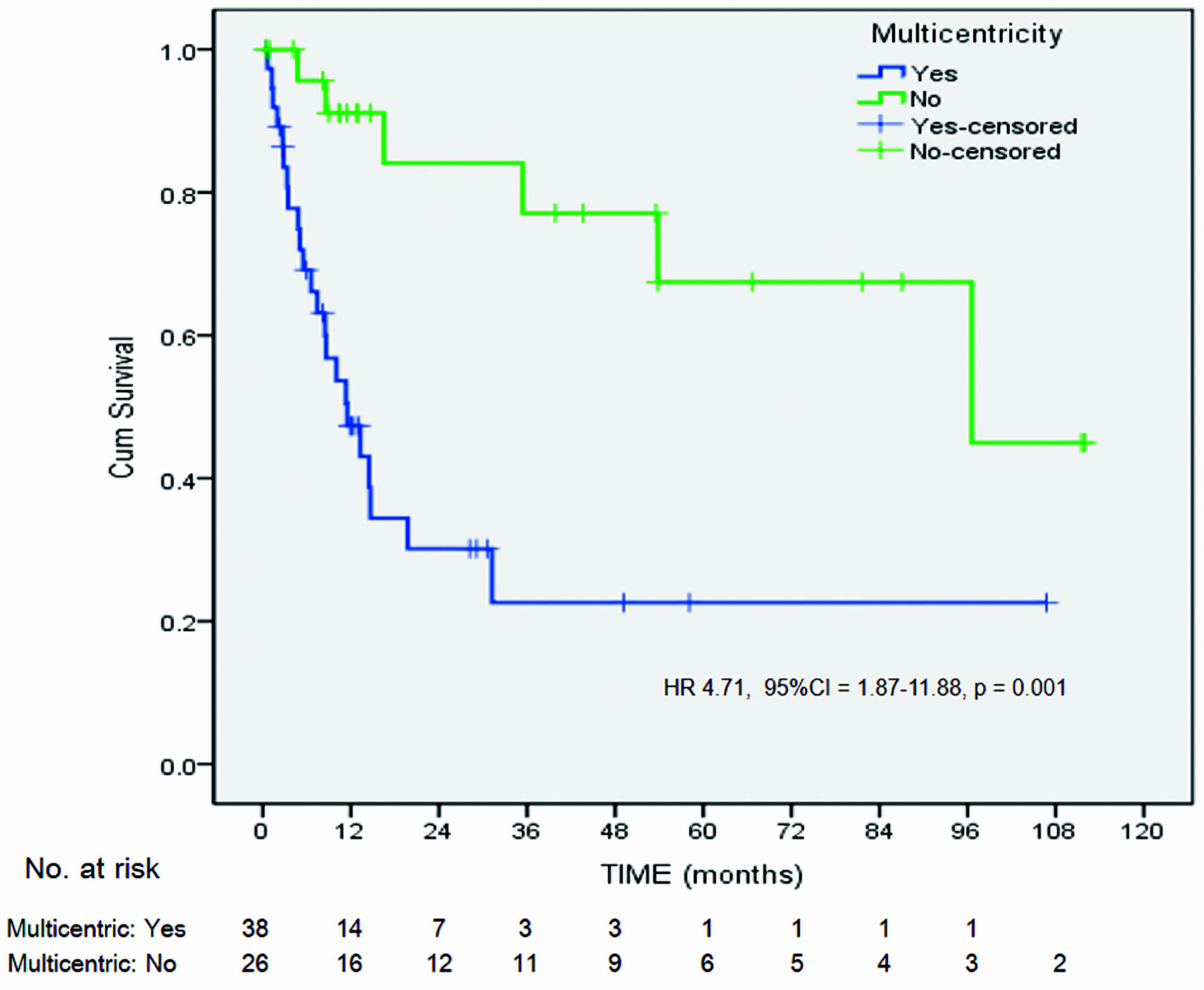 Click for large image | Figure 2. Kaplan-Meier life table analysis of recurrence-free survival in high-grade VIN/VAIN patients following laser vaporization, comparing patients with multicentricity and patients with unicentricity (log-rank P = 0.00035). HR: hazard ratio; CI: confidence interval; VIN: vulvar intraepithelial neoplasia; VAIN: vaginal intraepithelial neoplasia. |
 Click to view | Table 3. Risk Factors for High-Grade VAIN/VIN Recurrence/Persistence |
The authors obtained different results when analyzing those patients using the alternative definition (Table 3, Fig. 3). Multicentric IN was present in 22(33.8%) patients. Patients with multicentric IN had a recurrence/persistence rate of 43.1 per 100 person-years with a median time to recurrence/persistence of 14.6 months (95% CI: 7.7 - 21.6 months), while patients without this feature had a recurrence/persistence rate of 17.7 per 100 person-years with a median time to recurrence/persistence of 53.8 months (95% CI: 0.0 - 122.4 months, P = 0.0298). However, in contrast to the prior outcome derived from the main definition, there was no significant difference in RFS between the multicentric IN and unicentric groups (P = 0.143) (Fig. 3). In addition, univariate analysis revealed that recurrence/persistence was not associated with the presence of multicentric IN (P = 0.58) (Table 3).
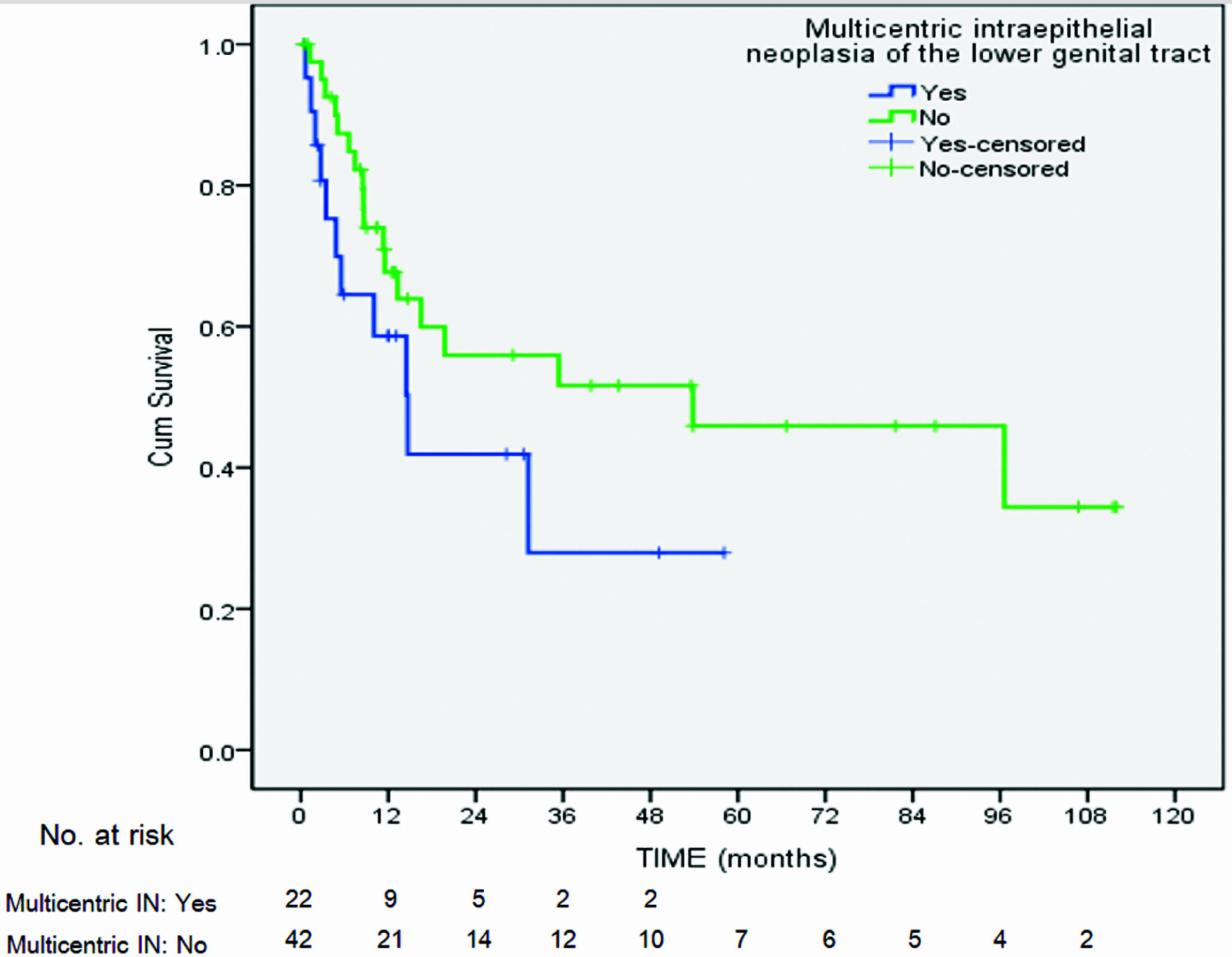 Click for large image | Figure 3. Kaplan-Meier life table analysis of recurrence-free survival in high-grade VIN/VAIN patients following laser vaporization, comparing patients with multicentric intraepithelial neoplasia with unicentric intraepithelial neoplasia (log-rank P = 0.143). VIN: vulvar intraepithelial neoplasia; VAIN: vaginal intraepithelial neoplasia. |
| Discussion | ▴Top |
The present study describes the results of laser vaporization and the associations of multicentricity and other risk factors with recurrence/persistence in patients with high-grade VIN/VAIN in a tertiary referral hospital. The recurrence/persistence rate following laser vaporization was 22.3 per 100 person-years, with a median time to recurrence/persistence of 31.2 months, which was in accordance with the findings of two previous reports [8, 20]. In a retrospective study of high-grade VIN/VAIN by Fehr et al, the recurrence rate was 24% after surgical biopsy combined with CO2 laser vaporization; however, there was a predominance of high-grade VIN in this study [8]. A randomized controlled trial by von Gruenigen et al reported a similar recurrence rate of 25.5% in patients with VIN/VAIN after CO2 laser vaporization, but patients with intraepithelial neoplasia grade 1 (IN1) were included in their trial [20]. Beavis et al evaluated patients with high-grade VIN/VAIN, and slightly more cases (28.6%) experienced recurrence during the median follow-up period of 29 months; nearly half of these patients had prior vulvovaginal high-grade squamous intraepithelial lesion (HSIL) treatment, and about one-third were current smokers [21]. Hillemanns et al reported a high recurrence rate of 40% after CO2 laser vaporization in patients with VIN (including patients with vulvar intraepithelial neoplasia grade 1 (VIN1)) over a long follow-up period of 53 months [7]. Wallbillich et al reported a higher recurrence rate associated with laser ablation (45%) compared to cold knife excision (26.7%) for treating vulvar intraepithelial neoplasia grade 2 or 3 (VIN2/3), but it was not inferior in terms of RFS [10]. Regarding laser vaporization for treatment of VAIN, some retrospective studies have reported recurrence rates of 38-50% for all grades of VAIN [5, 11], while recurrence rates for high-grade VAIN vary among studies from 0% to 43% [9, 12, 19]. Late recurrences can occur even at several years after the initial treatment [14]. Our patients had an increase in recurrence even at the end of the follow-up. The RFS rate at 1 year was 65.3%, but at 5 years, it had dropped to 41.6%. Our results are consistent with the results of a previous study that demonstrated that the RFS rate in laser-treated patients dropped from 62.2% at 1 year to 51.3% at 5 years, while the RFS rate was unchanged for the surgery group [4].
Overall, the evidence showed that surgical excision and laser vaporization were probably equally effective for treating vulvar HSIL. A study by van Esch et al reported recurrence rates of 48.8% and 56% in the excision and laser vaporization groups, respectively, but multivariate analysis revealed no difference in RFS according to treatment type [6]. However, high-quality evidence comparing the effectiveness of laser vaporization with excision is lacking [2]. In practice, larger, multifocal, or multicentric lesions are more likely to be treated with laser vaporization in order to maintain normal vulvovaginal anatomy and function; this was probably associated with increased recurrence in laser-treated patients compared with those undergoing excision [1].
In the current study, we analyzed the association between multicentricity and therapeutic outcomes, as we had observed a high incidence of multicentricity of the lower genital tract, accounting for 58% of cases. This finding corresponded with those of other studies that demonstrated that approximately 50-90% of cases had evidence of multicentricity of the lower genital tract [4-7, 11, 19]. In the present study, laser vaporization in cases with multicentricity had a significantly higher recurrence/persistence rate and lower RFS compared to cases with unicentricity. Several authors have identified multicentricity as a risk factor for recurrence [1, 4, 7, 13, 14]. There are limited data available in the literature regarding the characteristics and causes of this condition [16-18, 22]; however, multicentric lower genital tract disease may evolve through various pathways, such as a high susceptibility to HPV infections and HPV-induced development of distant, independent lesions or the “field effect” of infections involving high-risk HPV types [1, 16, 18]. Vinokurova et al suggested that a local dissemination of a preexisting monoclonal dysplastic cell clone originating at the cervical transformation zone is a cause of multicentric high-grade precancerous disease in the female lower genital tract [17]. In susceptible hosts, these cell clones can persist for a long time, culminating in a high recurrence rate [17, 18]. Categorizing these patients according to multicentric status would provide a risk-based approach to improve therapeutic benefits. Multicentricity status can be used to triage patients in need of highly experienced management and prolonged follow-up.
The theory of multicentric origin in multiple squamous cell carcinomas involving the cervix, vagina, and vulva were described by many authors a long time ago [23, 24]. Although the concept of multicentric lower genital tract disease is generally accepted, there are some variations or inconsistencies regarding the definition of multicentricity. Several previous studies have defined multicentricity as intraepithelial lesions of two or three sites in lower genital tract, excluding invasive lesions [4, 7, 14, 16, 18]. Other research has included any grade of IN or invasive lesions [17, 22, 25]. Another study has specifically included low-grade, high-grade and microinvasive lesion while excluding invasive lesion [13]. The authors therefore evaluated the clinical impact due to the variation of definition by comparing two types of definition. The alternative definition that excluded invasive cancer failed to demonstrate the effect of multicentric lower genital tract disease on the RFS and risk of recurrence/persistence. One of possible explanations regarding this is that the group of patients without feature of multicentric IN had more proportion of invasive lesions than group of patients without feature of multicentricity, rendering outcome inferior. Besides, the group of patients with feature of multicentric IN had less proportion of “previous neoplasia” compared to the group of patients with feature of multicentricity. Regarding this factor, as compared to “concurrent neoplasia” (synchronous), previous neoplasia (metachronous) potentially has a higher probability of recurrence, since those lesions have longer latent period for recurrence by the time of diagnosis, although this factor was not found to be the significant risk factor for recurrence/persistence in our analysis. However, it is not possible to make a valid comparison between metachronous group and synchronous group because of small sample size and patients’ selection.
We also found that a history of radiation and laser for recurrent cases after non-laser therapy were risk factors for recurrence/persistence, with approximately 6.3- and 5.3-fold increased risks, respectively; however, the number of cases at risk was small.
One of the strengths of our study was its specific aim of evaluating laser vaporization in patients with high-grade IN, particularly those with multicentricity, while previous studies have reported associations between multicentricity and outcomes for all treatment methods together [4, 7, 13, 14]. To the best of our knowledge, the present study is the first to demonstrate that in patients with high-grade VIN/VAIN treated with laser vaporization (which has unique characteristics compared to other treatments studied), multicentricity increased the risk of recurrence/persistence. Despite the small number of subjects (owing to the low incidence of the disease), the association of multicentricity was very highly significant. There were several limitations in this study. First, its retrospective design rendered the completeness of data impossible. Second, the small sample size due to the limited population rendered the outcomes difficult to interpret. In addition, data regarding HPV status and ancillary staining with p16 antibody were lacking. In the retrospective study with long period of data collection, the patients identified in this study were in the period before widespread use of HPV test and immunohistochemistry in our country. Our resource setting at the time of study period precluded using both tests in routine colposcopy service. Finally, the long period of data collection might have led to heterogeneity of clinical parameters related to evolving diagnostic criteria, definitions, and treatment techniques. There was also a lack of diagnostic criteria for differentiated VIN (dVIN), despite its high malignancy potential [1, 3], during the entire follow-up period.
Conclusions
Treatment of high-grade VIN/VAIN with laser vaporization depends on some prognostic risk factors which define the outcome. Multicentric disease is strongly associated with high treatment failure, with approximately half of patients having recurrence/persistence. Categorizing patients according to multicentric status would provide a risk-based approach to improve therapeutic benefits. Long-term follow-up is necessary as we found increasing recurrence even many years after the initial treatment.
Acknowledgments
The authors thank associate professor Dusit Sujirarat as the statistical consultant.
Financial Disclosure
There was no specific funding source to be mentioned.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Not applicable.
Author Contributions
Sathone Boonlikit: design, planning, conduct, data analysis, and manuscript writing. Punyacha Tangterdchanakit: conduct, data analysis, and manuscript writing - original draft.
Data Availability
The data that support the findings of this study are available from the corresponding author, Sathone Boonlikit, upon reasonable request.
Abbreviations
Anti-HIV: antibody to human immune deficiency virus; ASC-H: atypical squamous cells, high-grade squamous intraepithelial lesion cannot be excluded; ASC-US: atypical squamous cells of undetermined significance; CO2 laser: carbon dioxide laser; CIN: cervical intraepithelial neoplasia; CIN2/3: cervical intraepithelial neoplasia grade 2 or 3; CI: confidential interval; dVIN: differentiated vulvar intraepithelial neoplasia; high-grade IN+: high-grade intraepithelial neoplasia or worse; HSIL: high-grade squamous intraepithelial lesion; HPV: human papilloma virus; IN: intraepithelial neoplasia; HR: hazard ratio; IN2: intraepithelial neoplasia grade 2; IN3: intraepithelial neoplasia grade 3; LSIL: low-grade squamous intraepithelial lesion; OR: odds ratio; RFS: recurrence-free survival; VAIN: vaginal intraepithelial neoplasia; VAIN1: vaginal intraepithelial neoplasia grade 1; VAIN2: vaginal intraepithelial neoplasia grade 2; VAIN3: vaginal intraepithelial neoplasia grade 3; VIN: vulvar intraepithelial neoplasia; VIN1: vulvar intraepithelial neoplasia grade 1; VIN2: vulvar intraepithelial neoplasia grade 2; VIN2/3: vulvar intraepithelial neoplasia grade 2 or 3; VIN3: vulvar intraepithelial neoplasia grade 3
| References | ▴Top |
- Campion MJ, Canfell K. Preinvasive disease. In: Berek JS, Hacker NF, eds. Berek & Hacker's gynecologic oncology. 7th ed. Philadelphia: Wolters Kluwer. 2021; p. 222-308.
- Lawrie TA, Nordin A, Chakrabarti M, Bryant A, Kaushik S, Pepas L. Medical and surgical interventions for the treatment of usual-type vulval intraepithelial neoplasia. Cochrane Database Syst Rev. 2016;2016(1):CD011837.
doi pubmed pmc - Preti M, Joura E, Vieira-Baptista P, Van Beurden M, Bevilacqua F, Bleeker MCG, Bornstein J, et al. The European Society of Gynaecological Oncology (ESGO), the International Society for the Study of Vulvovaginal Disease (ISSVD), the European College for the Study of Vulval Disease (ECSVD) and the European Federation for Colposcopy (EFC) Consensus Statements on Pre-invasive Vulvar Lesions. J Low Genit Tract Dis. 2022;26(3):229-244.
doi pubmed pmc - Leufflen L, Baermann P, Jr., Rauch P, Routiot T, Bezdetnava L, Guillemin F, Desandes E, et al. Treatment of vulvar intraepithelial neoplasia with CO(2) laser vaporization and excision surgery. J Low Genit Tract Dis. 2013;17(4):446-451.
doi pubmed - Lenehan PM, Meffe F, Lickrish GM. Vaginal intraepithelial neoplasia: biologic aspects and management. Obstet Gynecol. 1986;68(3):333-337.
doi pubmed - van Esch EM, Dam MC, Osse ME, Putter H, Trimbos BJ, Fleuren G, van der Burg SH, et al. Clinical characteristics associated with development of recurrence and progression in usual-type vulvar intraepithelial neoplasia. Int J Gynecol Cancer. 2013;23(8):1476-1483.
doi pubmed - Hillemanns P, Wang X, Staehle S, Michels W, Dannecker C. Evaluation of different treatment modalities for vulvar intraepithelial neoplasia (VIN): CO(2) laser vaporization, photodynamic therapy, excision and vulvectomy. Gynecol Oncol. 2006;100(2):271-275.
doi pubmed - Fehr MK, Baumann M, Mueller M, Fink D, Heinzl S, Imesch P, Dedes K. Disease progression and recurrence in women treated for vulvovaginal intraepithelial neoplasia. J Gynecol Oncol. 2013;24(3):236-241.
doi pubmed pmc - Tainio K, Jakobsson M, Louvanto K, Kalliala I, Paavonen J, Nieminen P, Riska A. Randomised trial on treatment of vaginal intraepithelial neoplasia-Imiquimod, laser vaporisation and expectant management. Int J Cancer. 2016;139(10):2353-2358.
doi pubmed - Wallbillich JJ, Rhodes HE, Milbourne AM, Munsell MF, Frumovitz M, Brown J, Trimble CL, et al. Vulvar intraepithelial neoplasia (VIN 2/3): comparing clinical outcomes and evaluating risk factors for recurrence. Gynecol Oncol. 2012;127(2):312-315.
doi pubmed pmc - Dodge JA, Eltabbakh GH, Mount SL, Walker RP, Morgan A. Clinical features and risk of recurrence among patients with vaginal intraepithelial neoplasia. Gynecol Oncol. 2001;83(2):363-369.
doi pubmed - Bogani G, Ditto A, Martinelli F, Mosca L, Chiappa V, Rossetti D, Leone Roberti Maggiore U, et al. LASER treatment for women with high-grade vaginal intraepithelial neoplasia: A propensity-matched analysis on the efficacy of ablative versus excisional procedures. Lasers Surg Med. 2018;50(9):933-939.
doi pubmed - Ait Menguellet S, Collinet P, Houfflin Debarge V, Nayama M, Vinatier D, Leroy JL. Management of multicentric lesions of the lower genital tract. Eur J Obstet Gynecol Reprod Biol. 2007;132(1):116-120.
doi pubmed - Satmary W, Holschneider CH, Brunette LL, Natarajan S. Vulvar intraepithelial neoplasia: Risk factors for recurrence. Gynecol Oncol. 2018;148(1):126-131.
doi pubmed - Jamieson A, Tse SS, Brar H, Sadownik LA, Proctor L. A systematic review of risk factors for development, recurrence, and progression of vulvar intraepithelial neoplasia. J Low Genit Tract Dis. 2022;26(2):140-146.
doi pubmed - Zhang J, Liu G, Cui X, Yu H, Wang D. Human papillomavirus genotypes and the risk factors associated with multicentric intraepithelial lesions of the lower genital tract: a retrospective study. BMC Infect Dis. 2021;21(1):554.
doi pubmed pmc - Vinokurova S, Wentzensen N, Einenkel J, Klaes R, Ziegert C, Melsheimer P, Sartor H, et al. Clonal history of papillomavirus-induced dysplasia in the female lower genital tract. J Natl Cancer Inst. 2005;97(24):1816-1821.
doi pubmed - Hampl M, Wentzensen N, Vinokurova S, von Knebel-Doeberitz M, Poremba C, Bender HG, Kueppers V. Comprehensive analysis of 130 multicentric intraepithelial female lower genital tract lesions by HPV typing and p16 expression profile. J Cancer Res Clin Oncol. 2007;133(4):235-245.
doi pubmed - Hodeib M, Cohen JG, Mehta S, Rimel BJ, Walsh CS, Li AJ, Karlan BY, et al. Recurrence and risk of progression to lower genital tract malignancy in women with high grade VAIN. Gynecol Oncol. 2016;141(3):507-510.
doi pubmed - von Gruenigen VE, Gibbons HE, Gibbins K, Jenison EL, Hopkins MP. Surgical treatments for vulvar and vaginal dysplasia: a randomized controlled trial. Obstet Gynecol. 2007;109(4):942-947.
doi pubmed - Beavis A, Najjar O, Murdock T, Abing A, Fader A, Wethington S, Stone R, et al. Treatment of vulvar and vaginal dysplasia: plasma energy ablation versus carbon dioxide laser ablation. Int J Gynecol Cancer. 2021;31(11):1410-1415.
doi pubmed pmc - Gonzalez-Bosquet E, Mazarico E, Lorente N, Gomez-Roig MD. Risk factors to develop multicentric lesions of the lower genital tract. Eur J Gynaecol Oncol. 2017;38(1):10-13.
pubmed - Hammond IG, Monaghan JM. Multicentric carcinoma of the female lower genital tract. Br J Obstet Gynaecol. 1983;90(6):557-561.
doi pubmed - Marcus SL. Multiple squamous cell carcinomas involving the cervix, vagina, and vulva: the theory of multicentric origin. Am J Obstet Gynecol. 1960;80:802-812.
doi pubmed - Campion MJ, Singer A. Vulval intraepithelial neoplasia: clinical review. Genitourin Med. 1987;63(3):147-152.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Oncology is published by Elmer Press Inc.


