| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://www.wjon.org |
Original Article
Volume 15, Number 5, October 2024, pages 784-791
Assessment of Five-Year Relative Survival of Patients With Endometrial Cancer: A Period Analysis
Xiao Jiao Zhaoa, h, Xin Bingb, c, h, Qi Qi Leib, d, Yong Ran Chenge, Jun Yangc, Liang You Wangf, Tian Hua Cheng, i, Tian Hui Chenb, d, i
aDepartment of Medical Insurance, The Second Affiliated Hospital of Guizhou University of Traditional Chinese Medicine, Guiyang, China
bDepartment of Cancer Prevention, Zhejiang Cancer Hospital, Hangzhou 310022, China
cSchool of Public Health, Hangzhou Normal University, Hangzhou 311121, China
dHangzhou Institute of Medicine (HIM), Chinese Academy of Sciences, Hangzhou 310018, China
eSchool of Public Health, Hangzhou Medical College, Hangzhou, China
fDepartment of Non-communicable Chronic Disease Control and Prevention, Taizhou Municipal Center for Disease Control and Prevention, Taizhou 318000, Zhejiang Province, China
gDepartment of Neurology I, The First People’s Hospital of Hangzhou Lin’an District, Affiliated Lin’an People’s Hospital, Hangzhou Medical College, Hangzhou 311399, China
hThese authors contributed equally to this work.
iCorresponding Author: Tian Hua Chen, Department of Neurology I, The First People’s Hospital of Hangzhou Lin’an District, Affiliated Lin’an People’s Hospital, Hangzhou Medical College, Hangzhou 311399, China; Tian Hui Chen, Department of Cancer Prevention, Zhejiang Cancer Hospital, Hangzhou 310022, China
Manuscript submitted June 26, 2024, accepted July 23, 2024, published online August 10, 2024
Short title: Five-Year Relative Survival for Endometrial Cancer
doi: https://doi.org/10.14740/wjon1921
| Abstract | ▴Top |
Background: Endometrial cancer is one of the most common female cancers globally and in China. Although timely assessment of 5-year relative survival is crucial for guiding secondary prevention and early screening programs for endometrial cancer patients, those kinds of data are scarce in China. We aimed to provide a timely and accurate assessment of 5-year relative survival for patients with endometrial cancer from eastern China.
Methods: Overall, 945 patients diagnosed with endometrial cancer during 2004 - 2018 from four cancer registries with high-quality data from Taizhou, eastern China were included. Period analysis was used to calculate 5-year relative survival for overall and the stratification by age at diagnosis and region. Model-based period analysis was used to predict the 5-year relative survival for the upcoming period of 2019 - 2023.
Results: We found that 5-year relative survival during 2014 - 2018 reached 86.4% for overall, while urban areas had higher survival compared to rural areas (91.3% vs. 85.3%). Furthermore, there was a clear age gradient, decreasing from 89.3% for age < 55 years to 80.5% for age > 74 years. Predicted 5-year relative survival for the upcoming period 2019 - 2023 could reach 88.4%.
Conclusions: We provide, a timely and accurate assessment of 5-year relative survival for patients with endometrial cancer from Taizhou, eastern China, reaching 86.4% for overall. Our finding has important implications for the overall evaluation of early detection and screening programs for patients with endometrial cancer in eastern China.
Keywords: Endometrial cancer; 5-year relative survival; Cancer registry; Period analysis
| Introduction | ▴Top |
Endometrial cancer is a group of epithelial malignant tumors that occur in the endometrium. According to the Global Cancer Statistics 2020, there were 417,000 new endometrial cancer cases and 97,000 related deaths in 2020, making it the second most common cancer of the female reproductive system [1]. In 2015, there were 63,000 new cases and 22,000 deaths due to endometrial cancer in China [2]. From 2010 to 2014, endometrial cancer ranked eighth in terms of cancer incidence and 13th in terms of mortality among women in Zhejiang Province, China, with incidence and mortality rates of 9.46 and 2.72 per 100,000 women, respectively [3]. In Taizhou, the incidence of endometrial cancer increased from 4.73 per 100,000 women in 2010 to 7.69 per 100,000 women in 2016, with a rapid increase in incidence and a trend toward younger age of onset, posing a significant threat to women’s health [4].
Population-based cancer registration enables regular monitoring of cancer incidence, mortality, and prognosis. A key indicator for evaluating cancer prognosis is the relative survival, such as the 5-year relative survival. Currently, there are various methods for evaluating the 5-year relative survival of tumors, including the cohort method, complete method, and period analysis [5]. The period analysis was initially proposed by Professor Brenner in 1996, and in 2006, he proposed a model-based period analysis to predict the long-term survival of cancer patients in the upcoming years [6, 7]. The period analysis has been widely used in Europe and has become the “gold standard” for evaluating the 5-year relative survival of cancer [8-10]. Studies have demonstrated that the period analysis is superior to the traditional cohort method as it provides timely and accurate 5-year relative survival for cancer patients [11]. Our group confirmed, for the first time in China using period analysis, the superiority of the period analysis over the cohort method for endometrial cancer patients during 2009 - 2013 since 5-year relative survival estimated by period analysis (89.6%) was much closer to the observed survival (88.6%), compared to those estimated by traditional cohort method (79.4%) [5].
Although timely evaluation of the long-term survival of endometrial cancer is crucial for guiding secondary prevention and early screening programs, data are scarce on the 5-year relative survival for endometrial cancer in China. Therefore, this study aimed to provide the most up-to-date (during 2014 - 2018) 5-year relative survival data for endometrial cancer patients from Taizhou, eastern China using period analysis and to predict future survival during the upcoming 2019 - 2023 period using the model-based period analysis and the survival data during three continuous periods (2004 - 2008, 2009 - 2013, and 2014 - 2018).
| Materials and Methods | ▴Top |
Data source
While data on patients diagnosed with endometrial cancer were provided by nine cancer registries in Taizhou, data from four of those registries (Luqiao, Yuhuan, Xianju, Wenling) were selected for further analyses based on the criterion of “death certificate only (DCO)” cases less than 13%, covering a total population of 2.6 million. Cases coded as C54-C55 were identified as endometrial cancer according to the International Classification of Diseases (ICD-10) and the International Classification of Oncology (ICD-O-3).
Follow-up and quality control
All cancer registries used a combination of active and passive follow-up to determine survival information of endometrial cancer patients, and follow-up information was updated until December 31, 2018 (Table 1). The patient selection process is illustrated in Figure 1. A total of 1,148 patients with endometrial cancer were initially enrolled in four cancer registries during 2004 - 2018. After careful examination, we excluded 26 cases with missed follow-up, 35 cases with unknown records, and 114 cases with DCO > 13% from the analyses. The quality of the remaining data was further evaluated using IARCcrgTools, resulting in the removal of 28 cases with logical errors. Overall, 945 eligible cases were included in the survival analyses, comprising 67 cases from 2004 to 2008, 389 cases from 2009 to 2013, and 489 cases from 2014 to 2018.
 Click to view | Table 1. Illustration of Data Used to Calculate the 5-Year Relative Survival Estimates for Patients Diagnosed in 2004 - 2008, 2009 - 2013, and 2014 - 2018 Periods by Period Analysis |
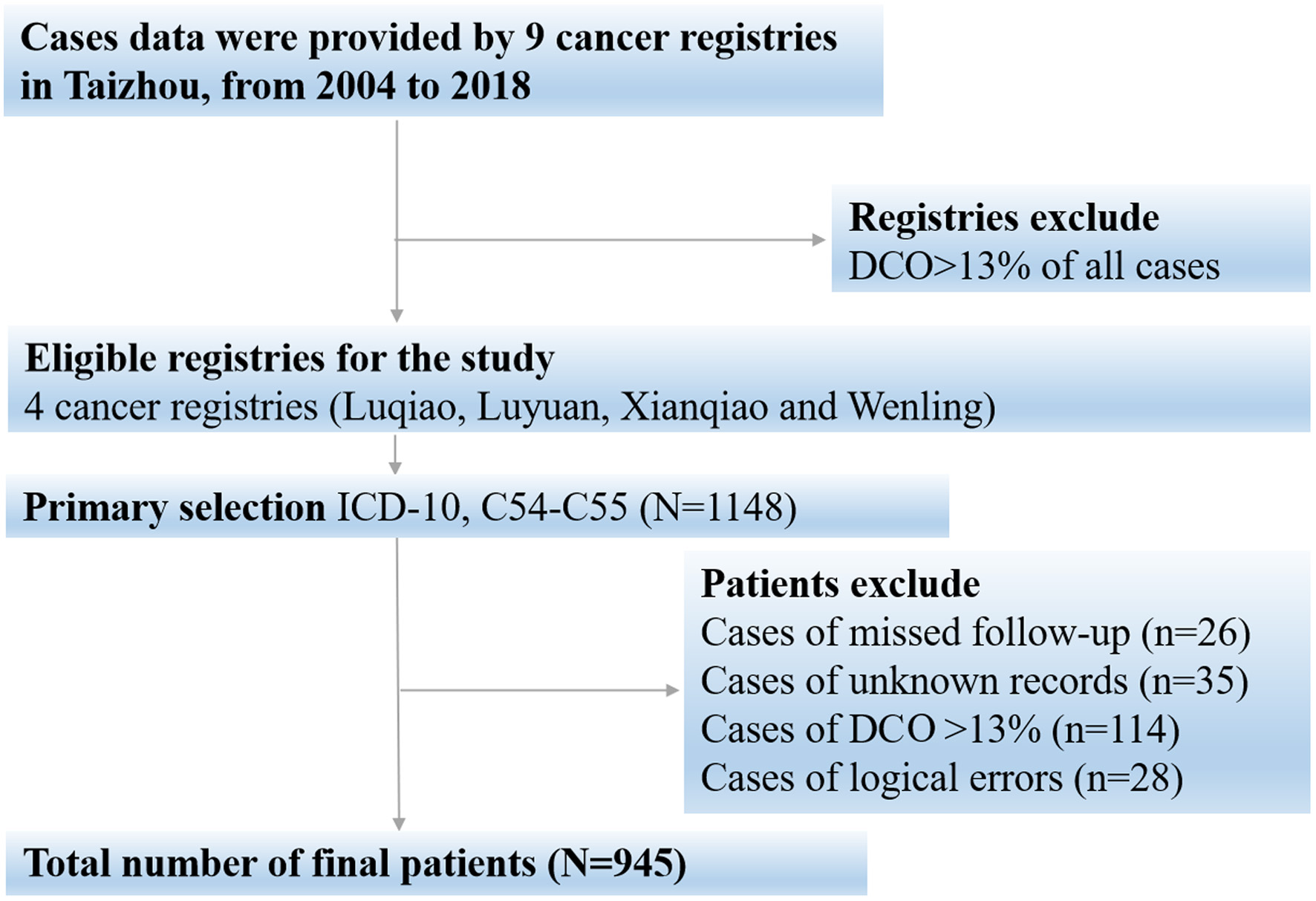 Click for large image | Figure 1. Flow chart for patient selection. |
Although the data from nine cancer registries from Taizhou, Eastern China were completely anonymous, and their use did not entail ethical problems, the data use for this study were approved and the written informed consent was also exempt by the Institutional Review Board of Zhejiang Cancer Hospital,China (IRB-2023-324).
Statistical analysis
The period analysis was used to calculate the 5-year relative survival for patients with endometrial cancer during 2014 - 2018. We used the “PeriodR” package for R version 3.13 software (R Foundation for Statistical Computing, Vienna, Austria) [12]. Specific steps are summarized below.
First, period analysis was used to calculate the 5-year relative survival for endometrial cancer patients during 2014 - 2018. This method required the handling of left-censored data diagnosed before the period of interest and right-censored data still alive after the end of the period of interest. The period analysis organized the data into a life table format and calculated the conditional 1-year survival for each follow-up year, expressed as:
In equation (1), ni represents the population at the beginning of the i year under follow-up, di represents the number of deaths at the end of the i year under follow-up, and ci represents the number of losses to follow-up during the i year. The observed survival for k years is obtained by multiplying the conditional 1-year survival for each year, expressed as:
The relative survival is the ratio of observed survival to expected survival, expressed as:
When calculating the 5-year relative survival, k = 5 in the equation. Sk represents the observed survival and S*k represents the expected survival. The expected survival is calculated using the Ederer II method. The point estimate and standard error of the relative survival are calculated using the Greenwood method.
We further predicted future survival during the upcoming 2019 - 2023 period using the model-based period analysis and the survival data during three continuous periods (2004 - 2008, 2009 - 2013, and 2014 - 2018). A generalized linear model was employed for the period analysis, which included cases diagnosed during three continuous periods (2004 - 2008, 2009 - 2013, and 2014 - 2018). The follow-up period and follow-up year were included as independent variables, with the conditional 1-year survival of each follow-up year as the dependent variable in the generalized linear model to predict the 5-year relative survival during the upcoming 2019 - 2023 period.
| Results | ▴Top |
Basic characteristics of endometrial cancer patients
Overall, 945 patients diagnosed with endometrial cancer were included in this study (Table 2). Rural areas had a higher proportion compared to urban areas (76.3% vs. 23.7%). The average age at diagnosis was 65.2 years. The distribution of patients across the four age groups was relatively balanced, while most patients were diagnosed between the ages of 65 and 74 years (32.9%).
 Click to view | Table 2. Basic Characteristics of Endometrial Cancer Patients Diagnosed During 2004 - 2018 From Taizhou, Eastern China |
Five-year relative survival during 2014 - 2018
Overall, 5-year relative survival during 2014 - 2018 reached 86.4%. Urban areas had higher 5-year relative survival compared to rural areas (91.3% vs. 85.3%). We found a clear age gradient, declining from 89.3% for patients younger than 55 years at diagnosis to 80.5% for those older than 74 years (Table 3).
 Click to view | Table 3. Five-Year Relative Survival of Endometrial Cancer Patients During 2014 - 2018 From Taizhou, Eastern China |
Five-year relative survival during the upcoming period 2019 - 2023
Using a model-based period analysis and the survival data during three continuous periods (2004 - 2008, 2009 - 2013 and 2014 - 2018), we predicted that overall 5-year relative survival for the forthcoming period 2019 - 2023 reached 88.4% (92.5% for urban areas and 87.3% for rural areas; Table 4).
 Click to view | Table 4. Predicted 5-Year Relative Survival for the Upcoming Period 2019 - 2023 for Endometrial Cancer Patients From Taizhou, Eastern China |
The trend of 5-year relative survival during 2004 - 2023
Over the past 15 years (2004 - 2018) and also for the upcoming 2019 - 2023 period, we observed an increasing trend in 5-year relative survival for overall and the stratification by region (Fig. 2). The trend was also consistent for the stratification by age at diagnosis (Fig. 3).
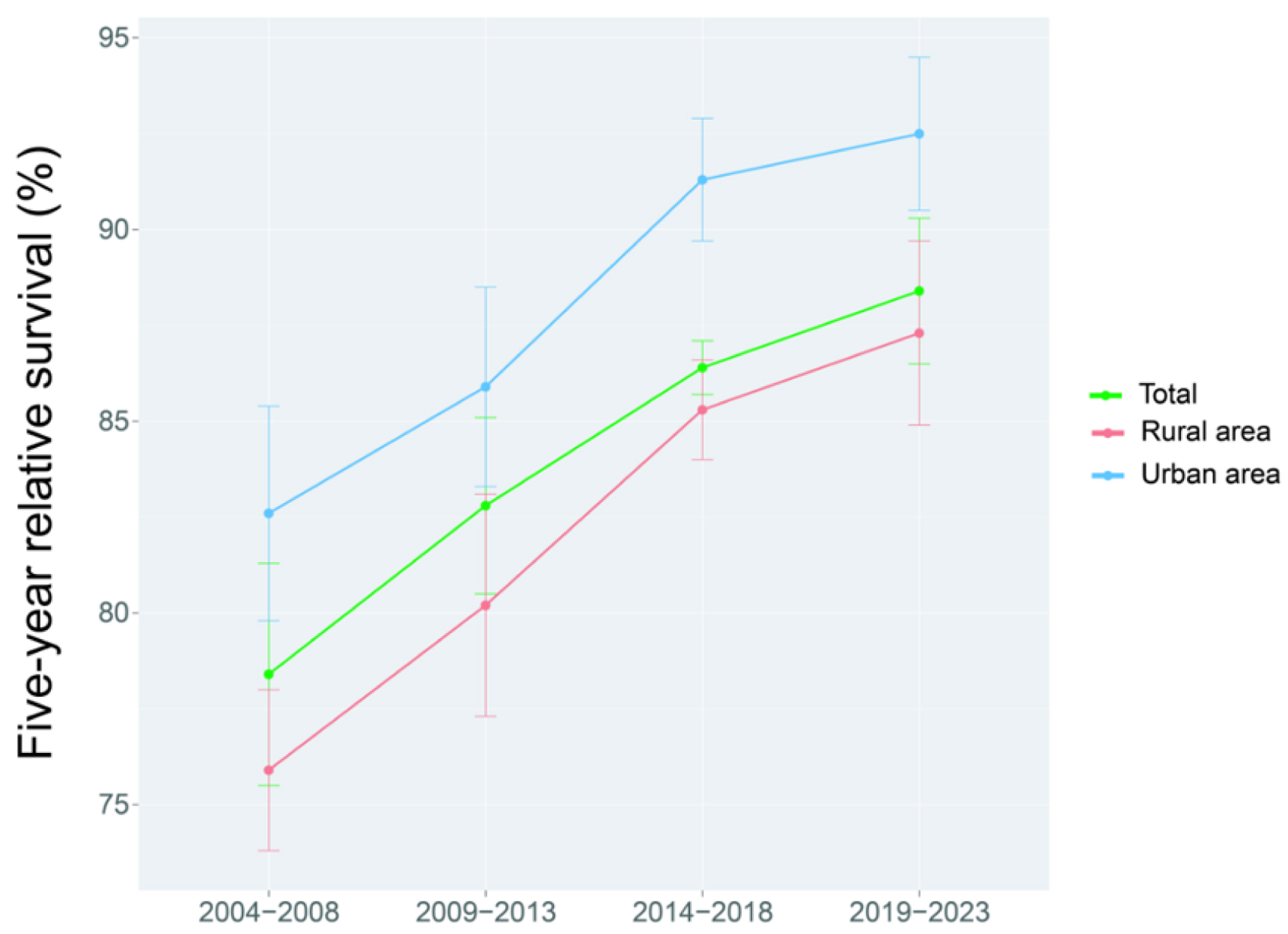 Click for large image | Figure 2. Trend of 5-year relative survival stratified by region for endometrial cancer patients from Taizhou, eastern China during 2004 - 2008, 2009 - 2013, 2014 - 2018 and 2019 - 2023. |
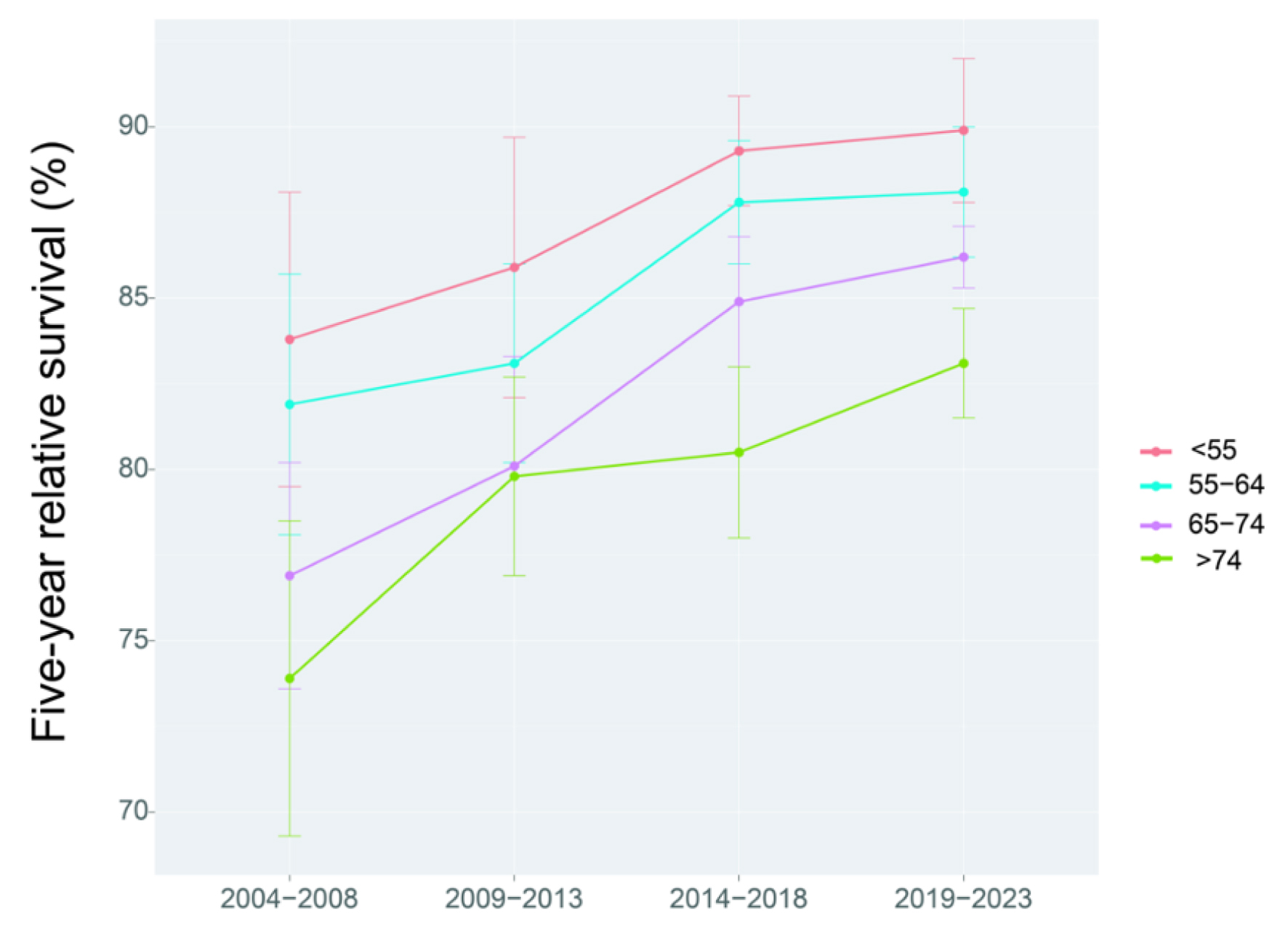 Click for large image | Figure 3. Trend of 5-year relative survival stratified by age at diagnosis for endometrial cancer patients from Taizhou, eastern China during 2004 - 2008, 2009 - 2013, 2014 - 2018 and 2019 - 2023. |
| Discussion | ▴Top |
To the best of our knowledge, this is the first study systematically using period analysis to provide the most up-to-date estimates of 5-year relative survival for endometrial cancer patients from Taizhou, eastern China, which reached 86% during 2014 - 2018 for overall. While urban areas had higher survival compared to rural areas (91.3% vs. 85.3%), we also observed a clear age gradient, which decreased from 89.3% for age at diagnosis < 55 years to 80.5% for age > 74 years. Additionally, we predicted that the 5-year relative survival for the upcoming period 2019 - 2023 could reach 88.4%, using the model-based period analysis and the survival data on the continuous three periods (2004 - 2008, 2009 - 2013 and 2014 - 2018). We observed an increasing trend in 5-year relative survival during 2004 - 2018 for overall and the stratification by region and age at diagnosis.
Endometrial cancer is generally associated with a favorable prognosis with a 5-year survival of roughly 80% due to its frequent early diagnosis and the efficacy of surgical treatments [13]. We found that 5-year relative survival for endometrial cancer patients from Taizhou, eastern China reached 86.4% during 2014 - 2018, which is higher than the report of 72.8% during 2012 - 2015 for China using only 17 cancer registries by Zeng et al and the report of 67.8% during 2011 - 2014 for Zhejiang Province [14, 15]. However, our results are plausible due to the below reasons. Firstly, Taizhou is located in the economically prosperous eastern coastal region of China, which has higher levels of medical investment compared to the national average. In contrast, the data on the Zeng et al study were obtained from 17 cancer registries and among them, 14 were from rural areas with limited resources, which could have contributed to a lower overall 5-year relative survival. Secondly, the report of 72.8% during 2012 - 2015 for China using only 17 cancer registries by Zeng et al [14] was a projected estimate, which is very likely underestimated because the survival data during 2003 - 2005 and 2006 - 2008 were calculated by cohort method, which must be under-estimated as confirmed by our group [5]. Lastly, the report of 67.8% during 2011 - 2014 for Zhejiang Province was 4 years early compared to our estimate of 86.4% during 2014 - 2018. Along with the advances in treatments of endometrial cancer patients in recent years [16, 17], the ongoing early screening programs for high-risk populations with endometrial cancer, and increased coverage of health insurance for endometrial cancer patients [18, 19], the 5-year relative survival for endometrial cancer patients from Taizhou, eastern China could be considerably improved.
From an international perspective, our findings are also consistent with the 5-year relative survival of endometrial cancer in Norway (86%) and the Netherlands (85%) [20, 21]. In Korea, the 5-year relative survival for endometrial cancer is nearly 90% [22], while in the United States [23] and Japan [24], the 5-year relative survival has already exceeded 90% which may reflect the positive impact of widespread screening programs and advanced medical care on the long-term survival of endometrial cancer patients from developed countries.
When stratified by region, we found rural areas had lower survival compared to urban areas (85.3% vs. 91.3%). The lower health literacy observed in rural areas can be attributed to socioeconomic disadvantages and a lack of comprehensive health education [25]. Several previous European studies have also confirmed socioeconomic deprivation’s impact on endometrial cancer survival rate [26, 27].
When stratified by age at diagnosis, we found a clear age gradient, decreasing from 89.3% for age at diagnosis < 55 years to 80.5% for age > 74 years, indicating that the age at diagnosis is an independent prognostic factor for endometrial cancer. Our finding is also consistent with a German multi-center retrospective study, which reports that the 5-year relative survival decreased from 90.0% for age at diagnosis 15 - 49 years to 74.8% for age at diagnosis > 70 years [28]. Another retrospective analysis carried out in Guangzhou province, China, also confirmed that elderly patients with endometrial cancer face a significantly worse prognosis compared to their younger counterparts [29]. The main reason is that elderly patients have more complications (e.g., diabetes and hypertension), a higher probability of special histological types and deep muscle infiltration, whereas younger patients with endometrial cancer primarily exhibit endometrioid adenocarcinoma histological types, superficial myometrial infiltration and demonstrate better tolerance to various treatment approaches [30, 31].
Moreover, endometrial cancer has entered the era of precision therapy at the molecular level, allowing for personalized treatment based on molecular subgroup stratification [32-34]. This has led to further improvements in long-term survival, thanks to advancements in genome mapping. Overall, with advancements in early detection, immune monotherapy, targeted therapy, and precision therapy, the prognosis for endometrial cancer has been improving. Continued research and advancements in these areas hold promise for further increasing long-term survival rates for patients.
Our study has several strengths and limitations. Firstly, throughout the study, we ensured the completeness and reliability of our data by strictly adhering to the relevant standards for data collection. Secondly, four cancer registries included in our study used a combination of active and passive follow-up methods to obtain the latest survival information for endometrial cancer patients. The utilization of active follow-up reduced the risk of inaccurate or lost-to-follow-up survival data, thereby greatly reducing the potential for overestimation or underestimation of real survival. Moreover, our method provides more timely and accurate long-term survival data compared to the traditional cohort method. Our study results can serve as baseline data for survival studies of endometrial cancer in Taizhou, eastern China. Nonetheless, our study does have two limitations. Firstly, due to the limited availability of detailed information in population-based cancer registries, we were unable to provide stratified data on histology, stage, and treatment for endometrial cancer patients. Secondly, our data exclusively encompass the population of Taizhou, eastern China, thereby potentially limiting its generalizability to the broader Chinese population. Therefore, future research could consider incorporating large-scale cancer registry data and necessitate the provision of comprehensive information on cancer staging and treatment methods by registry offices. By addressing these limitations, a more comprehensive understanding of endometrial cancer survival in China can be attained.
Conclusion
In summary, this study systematically using period analysis to provide the most up-to-date estimates of 5-year relative survival for endometrial cancer patients from Taizhou, eastern China, which reached 86% during 2014 - 2018 for overall. Our finding has important implications for the overall evaluation of early detection and screening programs for patients with endometrial cancer in eastern China.
Acknowledgments
None to declare.
Financial Disclosure
This work was supported by grants from National Key Research-Development Program of China (2019YFE0198800), Zhejiang Provincial Ten-Thousand Talents Plan “Leading Talents in Innovation on Science and Technology” (2021R52020), and Joint Key Program of Zhejiang Province-Ministry of Health (WKJ-ZJ-1714).
Conflict of Interest
None to declare.
Informed Consent
Written informed consent was exempted by the Institutional Review Board of Zhejiang Cancer Hospital, China (IRB-2023-324).
Author Contributions
THC was responsible for the study concept and design. LYW acquired data. YRC and QQL analyzed data. XJZ and XB drafted the manuscript, and all authors revised it for important intellectual content. All authors read and approved the final manuscript.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209-249.
doi pubmed - Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115-132.
doi pubmed - Zhao L, Chen Q, Shen P, Lin H, Du L. Incidence and mortality of corpus uteri cancer in Zhejiang cancer registration areas, 2010 to 2014. Chinese Journal of Cancer Prevention and Treatment. 2020;27(06):424-430.
- Qiao D, Wang L, Guo Y, Chai W, Li S, Liu L, Xie W. Incidence and mortality of corpus uteri cancer in Taizhou,2010-2016. Chinese Journal of Public Health Management. 2019;35(04):507-510.
- Jiang X, Wang L, Cheng Y, Tang H, Chen T. Assessment of long-term survival of cancer patients using cancer registry data from eastern China: Period analysis is superior to traditional methods. Int J Cancer. 2020;147(4):996-1005.
doi pubmed - Brenner H, Gefeller O. An alternative approach to monitoring cancer patient survival. Cancer. 1996;78(9):2004-2010.
pubmed - Brenner H, Hakulinen T. Up-to-date and precise estimates of cancer patient survival: model-based period analysis. Am J Epidemiol. 2006;164(7):689-696.
doi pubmed - Houterman S, Janssen-Heijnen ML, van de Poll-Franse LV, Brenner H, Coebergh JW. Higher long-term cancer survival rates in southeastern Netherlands using up-to-date period analysis. Ann Oncol. 2006;17(4):709-712.
doi pubmed - Talback M, Stenbeck M, Rosen M. Up-to-date long-term survival of cancer patients: an evaluation of period analysis on Swedish Cancer Registry data. Eur J Cancer. 2004;40(9):1361-1372.
doi pubmed - Jansen L, Hakulinen T, Brenner H. Study populations for period analyses of cancer survival. Br J Cancer. 2013;108(3):699-707.
doi pubmed pmc - Brenner H. Long-term survival rates of cancer patients achieved by the end of the 20th century: a period analysis. Lancet. 2002;360(9340):1131-1135.
doi pubmed - Holleczek B, Gondos A, Brenner H. periodR - an R package to calculate long-term cancer survival estimates using period analysis. Methods Inf Med. 2009;48(2):123-128.
doi pubmed - Amant F, Moerman P, Neven P, Timmerman D, Van Limbergen E, Vergote I. Endometrial cancer. Lancet. 2005;366(9484):491-505.
doi pubmed - Zeng H, Chen W, Zheng R, Zhang S, Ji JS, Zou X, Xia C, et al. Changing cancer survival in China during 2003-15: a pooled analysis of 17 population-based cancer registries. Lancet Glob Health. 2018;6(5):e555-e567.
doi pubmed - Li H, Du L, Li Q, Jiang C, Zhu Y, Yang J, Zhu C, Chen M. Cancer survival in Haining and Jiashan cancer registry areas of Zhejiang province. China Cancer. 2020;29(01):14-21.
- Forsse D, Berg HF, Bozickovic O, Engerud H, Halle MK, Hoivik EA, Woie K, et al. Maintained survival outcome after reducing lymphadenectomy rates and optimizing adjuvant treatment in endometrial cancer. Gynecol Oncol. 2021;160(2):396-404.
doi pubmed - van Weelden WJ, Reijnen C, Eggink FA, Boll D, Ottevanger PB, van den Berg HA, van der Aa MA, et al. Impact of different adjuvant treatment approaches on survival in stage III endometrial cancer: A population-based study. Eur J Cancer. 2020;133:104-111.
doi pubmed - Schiemer R, Furniss D, Phang S, Seddon AB, Atiomo W, Gajjar KB. Vibrational biospectroscopy: an alternative approach to endometrial cancer diagnosis and screening. Int J Mol Sci. 2022;23(9):4859.
doi pubmed pmc - Herzog C, Marin F, Jones A, Evans I, Reisel D, Redl E, Schreiberhuber L, et al. A simple cervicovaginal epigenetic test for screening and rapid triage of women with suspected endometrial cancer: validation in several cohort and case/control sets. J Clin Oncol. 2022;40(33):3828-3838.
doi pubmed pmc - Trovik J, Mauland KK, Werner HM, Wik E, Helland H, Salvesen HB. Improved survival related to changes in endometrial cancer treatment, a 30-year population based perspective. Gynecol Oncol. 2012;125(2):381-387.
doi pubmed - Boll D, Karim-Kos HE, Verhoeven RH, Burger CW, Coebergh JW, van de Poll-Franse LV, van Doorn HC. Increased incidence and improved survival in endometrioid endometrial cancer diagnosed since 1989 in The Netherlands: a population based study. Eur J Obstet Gynecol Reprod Biol. 2013;166(2):209-214.
doi pubmed - Shin DW, Jung KW, Ha J, Bae J. Conditional relative survival of patients with endometrial cancer: a Korean National Cancer Registry study. J Gynecol Oncol. 2022;33(2):e23.
doi pubmed pmc - Anderson C, Bae-Jump VL, Broaddus RR, Olshan AF, Nichols HB. Long-term patterns of excess mortality among endometrial cancer survivors. Cancer Epidemiol Biomarkers Prev. 2021;30(6):1079-1088.
doi pubmed pmc - Ito Y, Miyashiro I, Ito H, Hosono S, Chihara D, Nakata-Yamada K, Nakayama M, et al. Long-term survival and conditional survival of cancer patients in Japan using population-based cancer registry data. Cancer Sci. 2014;105(11):1480-1486.
doi pubmed pmc - Huang J, Deng Y, Boakye D, Tin MS, Lok V, Zhang L, Lucero-Prisno DE, 3rd, et al. Global distribution, risk factors, and recent trends for cervical cancer: A worldwide country-level analysis. Gynecol Oncol. 2022;164(1):85-92.
doi pubmed - Bedir A, Abera SF, Vordermark D, Medenwald D. Socioeconomic disparities in endometrial cancer survival in Germany: a survival analysis using population-based cancer registry data. J Cancer Res Clin Oncol. 2022;148(5):1087-1095.
doi pubmed pmc - Njoku K, Barr CE, Hotchkies L, Quille N, Wan YL, Crosbie EJ. Impact of socio-economic deprivation on endometrial cancer survival in the North West of England: a prospective database analysis. BJOG. 2021;128(7):1215-1224.
doi pubmed pmc - Chen T, Jansen L, Gondos A, Ressing M, Holleczek B, Katalinic A, Brenner H, et al. Survival of endometrial cancer patients in Germany in the early 21st century: a period analysis by age, histology, and stage. BMC Cancer. 2012;12:128.
doi pubmed pmc - Yang X, Li X. Effect of age of disease on the prognosis of endometrial cancer. Guangdong Medical Journal. 2015;36(07):1033-1036.
- Wright JD, Lewin SN, Barrena Medel NI, Sun X, Burke WM, Deutsch I, Herzog TJ. Endometrial cancer in the oldest old: Tumor characteristics, patterns of care, and outcome. Gynecol Oncol. 2011;122(1):69-74.
doi pubmed - Semaan A, Ali-Fehmi R, Munkarah AR, Bandyopadhyay S, Morris RT, Rizk S, Mert I, et al. Clinical/pathologic features and patient outcome in early onset endometrial carcinoma: a population based analysis and an institutional perspective from the Detroit metropolitan area, Michigan. Gynecol Oncol. 2012;124(2):265-269.
doi pubmed - van den Heerik A, Horeweg N, de Boer SM, Bosse T, Creutzberg CL. Adjuvant therapy for endometrial cancer in the era of molecular classification: radiotherapy, chemoradiation and novel targets for therapy. Int J Gynecol Cancer. 2021;31(4):594-604.
doi pubmed pmc - Bogani G, Giannini A, Vizza E, Di Donato V, Raspagliesi F. Sentinel node mapping in endometrial cancer. J Gynecol Oncol. 2024;35(1):e29.
doi pubmed pmc - Cuccu I, Raspagliesi F, Malzoni M, Vizza E, Papadia A, Di Donato V, Giannini A, et al. Sentinel node mapping in high-intermediate and high-risk endometrial cancer: Analysis of 5-year oncologic outcomes. Eur J Surg Oncol. 2024;50(4):108018.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Oncology is published by Elmer Press Inc.


