| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://www.wjon.org |
Original Article
Volume 14, Number 2, April 2023, pages 135-144
Improving Gastrointestinal Cancer Care by Enhanced Recovery Protocol Implementation
Lexi Frankela, Diego Maurenteb, Amalia D. Ardeljanb, Manjani Diveshb, Ali M. Rashidb, Kazuaki Takabec, d, Omar M. Rashida, b, e, f, g, h, i, j, k
aNova Southeastern University, Dr. Kiran C. Patel College of Allopathic Medicine, Fort Lauderdale, FL, USA
bMichael and Dianne Biennes Comprehensive Cancer Center, Holy Cross Health, Fort Lauderdale, FL, USA
cDepartment of Surgical Oncology, Roswell Park Comprehensive Cancer Center, Buffalo, NY, USA
dDepartment of Surgery, University at Buffalo Jacobs School of Medicine and Biomedical Sciences, the State University of New York, Buffalo, NY, USA
eUniversity of Miami, Leonard Miami School of Medicine, Miami, FL, USA
fMassachusetts General Hospital, Boston, MA, USA
gBroward Health, Fort Lauderdale, FL, USA
hTopLine MD Alliance, Fort Lauderdale, FL, USA
iMemorial Health, Pembroke Pines, FL, USA
jDelray Medical Center, Delray, FL, USA
kCorresponding Author: Omar M. Rashid, Complex General Surgical Oncology, General & Robotic Surgery, TopLine MD Alliance, Fort Lauderdale, FL 33308, USA
Manuscript submitted October 6, 2022, accepted February 24, 2023, published online March 24, 2023
Short title: Enhanced Recovery Protocol for GI Cancer
doi: https://doi.org/10.14740/wjon1534
| Abstract | ▴Top |
Background: Enhanced recovery protocols (ERPs) have become the standard of care for patients undergoing elective small bowel surgeries but have not yet been adequately studied in community hospitals. In this study, a multidisciplinary ERP was developed and implemented at a community hospital to include minimal anesthesia, early ambulation and enteral alimentation, and multimodal analgesia. The aim of this study was to determine the effects of the ERP on postoperative length of stay (LOS), readmission (RA) rates following bowel surgery, and postoperative outcomes.
Methods: The study design was a retrospective review of patients undergoing major bowel resection at Holy Cross Hospital (HCH) from January 1, 2017 to December 31, 2017. Patient charts for diagnostic-related group (DRG) 329, 330, and 331 were retrospectively reviewed at HCH in 2017 to compare outcomes in ERP versus non-ERP cases. The Medicare claims database (CMS) was also retrospectively reviewed to compare HCH data to the national average LOS and RA for the same DRG codes. Mean values for LOS and RA were statistically compared to determine significant differences between ERP versus non-ERP patients at HCH and national CMS data versus HCH patients.
Results: LOS was analyzed for each DRG at HCH. At HCH, for DRG 329, the mean LOS for non-ERP was 13.0833 days (n = 12) versus 3.375 days (n = 8) (P ≤ 0.001) for ERP. For DRG 330, the mean LOS for non-ERP was 10.861 days (n = 36) versus 4.583 days (n = 24) (P ≤ 0.001) for ERP. For DRG 331, the mean LOS for non-ERP was 7.272 days (n = 11) versus 3.348 days (n = 23) (P = 0.004) for ERP. LOS was also compared to national CMS data. The LOS at HCH for DRG 329 improved from the 10th to 90th percentile (n = 238,907); DRG 330 improved from the 10th to the 72nd percentile (n = 285,423); DRG 331 improved from 10th to 54th percentile (n = 126,941) (P < 0.001). The RA at HCH in ERP and non-ERP cases was 3% at 30 and 90 days. CMS RA for DRG 329 was 25.1% at 90 days and 9.9% at 30 days; DRG 330 RA was 18.3% at 90 days and 6.6% at 30 days; DRG 331 RA was 11% at 90 days and 3.9% at 30 days.
Conclusion: Implementation of ERP following bowel surgery at HCH significantly improved outcomes, in comparison to non-ERP cases, national CMS data, and Humana data. Further research on ERP for other fields and its impact on outcomes in other community settings is recommended.
Keywords: Enhanced recovery protocols; Length of stay; Readmission rate; HCH; MGH; CMS; Humana
| Introduction | ▴Top |
Enhanced recovery protocols (ERPs) include a multimodal perioperative care pathway proven to decrease recovery times and postoperative complication rates for patients undergoing major surgery [1]. ERP combines evidence-based perioperative interventions with multidisciplinary approaches in which healthcare professionals of different disciplines collaborate to achieve multiple elements of a protocol [2]. Prior ERP studies have demonstrated the improved survival and quality of life resulting from the perioperative effects of improved nutrition and metabolic function, reconciliation of patient expectations, enhanced performance status, and psychological wellbeing [2]. Standardized pathways for perioperative management have been shown to reduce postoperative length of stay (LOS) by more than 30% and postoperative complications by up to 50% [3]. This drastic reduction in LOS and complications also leads to a subsequent reduction in community healthcare costs [4].
ERP has been implemented successfully for several types of surgeries including coronary artery bypass, sigmoid resection, pancreaticoduodenectomy, among others [5-8]. More recently, ERPs have been studied for bowel cancer surgery and have also shown favorable postoperative outcomes. However, the postoperative outcomes reported in the literature seem to vary by institution. While some studies report a reduction in LOS [9-11] after ERP implementation, others show no difference in LOS [12]. Other reported benefits include an improvement in gastrointestinal function [12], receiving on-time adjuvant chemotherapy [13]. One recent study even demonstrates a postoperative reduction in narcotic use after implementation of an ERP at their institution [9]. Reduction in LOS has also been shown to vary depending on physician adherence to ERP, with larger reductions in LOS for providers more closely adhering to the ERP [14]. A recent meta-analysis studying gastrointestinal function after ERP implementation reports that the literature was too heterogeneous and precludes a meaningful result [15]. For this reason, single-institution studies may still be necessary to assess the function of an ERP on a smaller scale. Bowel cancer patients suffer from a high rate of physical debility and treatment-associated morbidity, resulting in high rates of malnutrition, hospital admissions, medical and perioperative complications [16, 17]. As current methods of postoperative management following bowel surgery are extremely costly, have not changed for several years, and lead to lengthy hospital stays, there is need for a prospective ERP design and its implementation across various institutions and healthcare systems [18]. A perioperative care pathway for all elective bowel surgery and bowel cancer surgery patients may thus lead to improved quality of life and decreased complications, LOS, and financial burden.
This elective bowel surgery ERP was developed by Holy Cross Hospital (HCH) in collaboration with Massachusetts General Hospital (MGH). It combines the successful elements of previous programs with a proactive and personalized approach to improve quality and reduce costs in community-based settings. In this study, all elective bowel surgery patients were offered an individualized intervention program based on a multidisciplinary assessment, integrating resources from physical therapy, social work, nutrition, spiritual services, acupuncture, alternative medicine, nursing, anesthesia and surgery. The aim of this study was to evaluate the clinical efficacy of this individualized perioperative ERP for patients undergoing elective bowel surgery and to compare outcomes based on postoperative morbidity, mortality, LOS, and readmission (RA) rates [4].
| Materials and Methods | ▴Top |
Study design
The study design was a retrospective review of patients undergoing major bowel resection at HCH from January 1, 2017 to December 31, 2017. LOS was compared between ERP and non-ERP participating patients by two methods. One method compared the LOS of ERP participating surgeons before (Fig. 1: pre, light blue bar) and after (Fig. 1: post, light blue bar) they implemented ERP into their practice. In this fashion, LOS was compared before and after ERP use among the same surgeons to reduce risk of user bias. The LOS of ERP versus non-ERP participating surgeons after implementation of ERP was then compared subsequently.
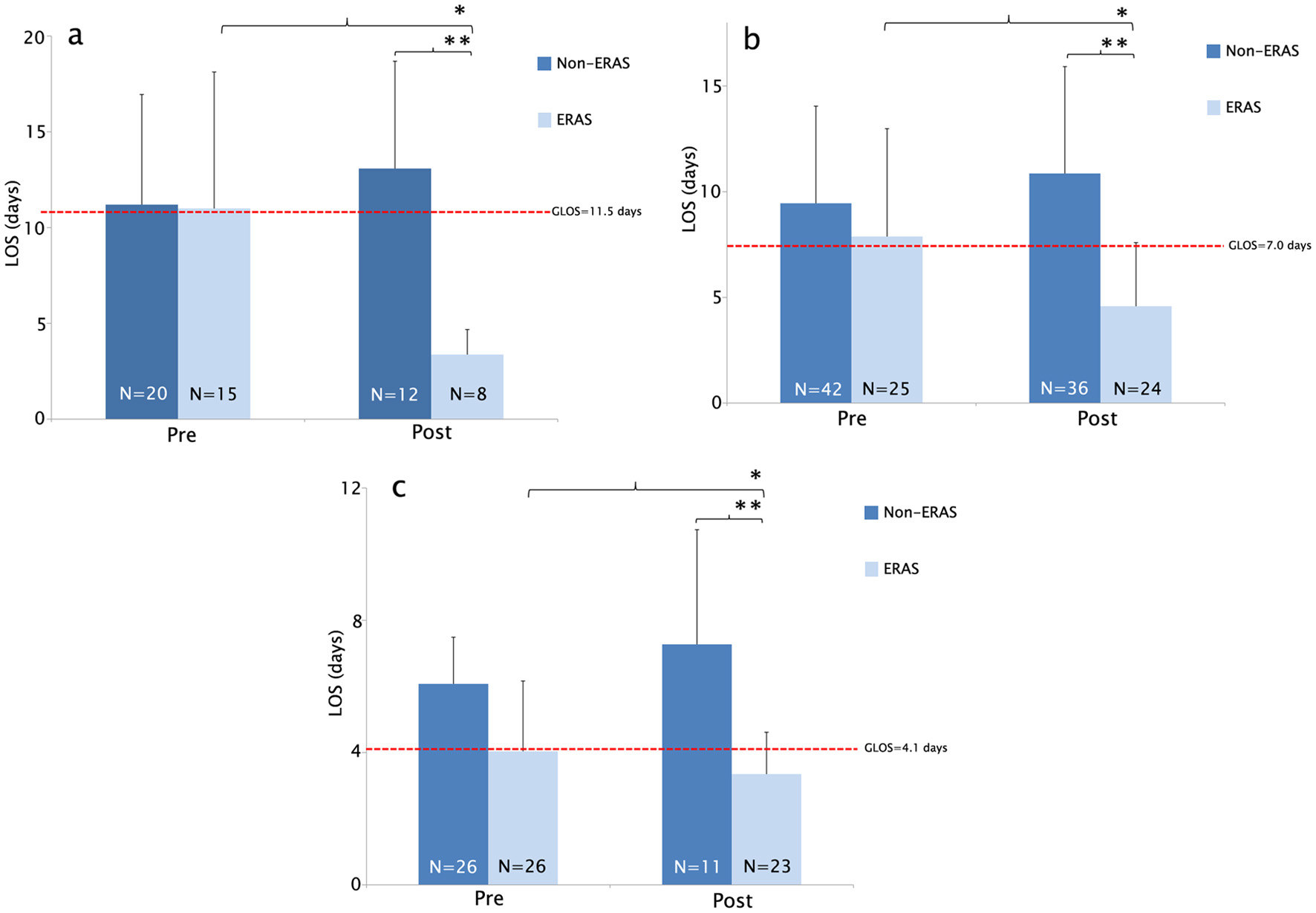 Click for large image | Figure 1. (a) Average LOS was significantly reduced in the ERP participating group DRG 329 at HCH. LOS significantly improved among ERP participating surgeons when compared before and after ERP implementation (*Reduction in LOS (days) 11.0 vs. 3.375, *P = 0.001). LOS significantly improved in patients undergoing ERP compared to patients undergoing non-ERP (**Reduction in LOS (days) 13.0833 vs. 3.375 (**P = 6.99 × 10-5)). (b) Average LOS was significantly reduced in the ERP participating group DRG 330 at HCH. LOS significantly improved among ERP participating surgeons when compared to before and after ERP implementation (*Reduction in LOS (days) 7.88 vs. 4.58 (*P = 0.008)). LOS significantly improved in patients undergoing ERP compared to patients undergoing non-ERP (**Reduction in LOS (days) 10.861 vs. 4.583 (**P = 1.31 × 10-7)). (c) Average LOS was significantly reduced in ERP participating group DRG 331 at HCH. LOS significantly improved among ERP participating surgeons when compared before and after ERP implementation (*Reduction in LOS (days) 4.03 vs. 3.34 (*P = 0.1689)). LOS significantly improved in patients undergoing ERP compared to patients undergoing non-ERP (**Reduction in LOS (days) 7.272 vs. 3.34 (**P = 0.004)). ERP: enhanced recovery protocol; DRG: diagnostic-related group; LOS: length of stay; HCH: Holy Cross Hospital. |
At HCH, a total number of 114 (ERP = 55 and non-ERP = 59) patients underwent major bowel surgery from January 1, 2017 to December 31, 2017. As demonstrated in Table 1, all ERP patients underwent a multidisciplinary multimodality regimen of standardized perioperative care. In contrast, non-ERP patients underwent care that was at the discretion of the providers on an ad hoc basis, other than the standard requirements set by quality and safety standards such as deep vein thrombosis (DVT) prophylaxis, infection control, etc. (Table 1). With the implementation of a multidisciplinary team to track outcomes and monitor adherence to ERP, all ERP patients were in compliance with the ERP perioperative program.
 Click to view | Table 1. Preoperative, Intraoperative, and Postoperative Care Protocols for the Patients Undergoing ERP and not Undergoing ERP |
The study was approved by IRB, and conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
Inclusion and exclusion criteria
Inclusion criteria consisted of patients undergoing major bowel resection at HCH, a small community hospital in Fort Lauderdale, Florida, consisting of patients with DRG 329, DRG 330, or DRG 331 documented into their records. The surgeon performing the bowel surgery decided whether or not to participate in the ERP for their patients.
Exclusion criteria consisted of patients undergoing emergency, urgent, or non-elective procedures. Patients not in compliance with the ERP were also included in the exclusion criteria, although no patients ended up meeting these criteria.
Data sources and study population
One hundred and fourteen patients undergoing major bowel resection (DRG 329, DRG 330, and DRG 331) at HCH, a small community hospital in Fort Lauderdale, Florida, were identified in this comparative analysis. Patients were stratified into two comparison groups: ERAS protocol (“ERP”, n = 55) and non-ERAS protocol (“non-ERP”, n = 59). Both groups were subject to preoperative, intraoperative, and postoperative care by the same group of board-certified surgeons.
A retrospective chart review was conducted for DRG 329, 330, and 331 at HCH between January 1, 2017 and December 31, 2017 and through a Health Insurance Portability and Accountability Act (HIPPA) compliant national database to compare outcomes in ERP versus non-ERP cases. Between January 1, 2007 and December 31, 2012, the CMS query resulted in a total number of 694,554 patients who underwent major bowel surgery. In the Medicare query, 238,907/651,271 patients underwent DRG 329, 285,423 underwent DRG 330, and 126,941 had major bowel surgery without comorbid conditions (DRG 331). The quest in Humana showed a total result of 43,283 cases. Of these, there were 13,286 for DRG 329, 19,370 for DRG 330, and 10,627 for DRG 331.
The national Medicare database contains demographics, procedure volume, and average cost information for each diagnostic-related group (DRG). Data queried for the present comparison were derived from the database between January 1, 2007 and December 31, 2012. For the purpose of this study, the database was queried for patients undergoing major bowel surgeries with or without major complications, or comorbid conditions, using the DRG codes mentioned in Table 2. Access to the database was granted from the provider for the purpose of academic research.
 Click to view | Table 2. DRG, 2007 - 2012, for Bowel Surgeries Which Were Utilized to Identify Cases for Chart Review |
Demographic information of study population
The gender distribution in the Medicare patient population showed that more females underwent major bowel surgery with a percentage of 59.60% and 40.40% males, while there was an approximately close result in Humana with 44.02% males and 54.98% females. Within both the Medicare and Humana populations, the regional distribution is represented with a high incidence of cases in the Southern United States followed by the Midwest, Northeast, and the West. In the Medicare database, the Charlson Comorbidity Index (CCI) ranges from 1 to 33 for DRG 329, with an average of 8 and median of 7. For DRG 330, CCI ranges from 1 to 32 with an average and median of 7. DRG 331 shows CCI ranges between 1 and 29 with an average and median of 6. In the Humana database, for DRG 329 CCI ranges from 0 to 29 with an average and median of 5. For DRG 330, CCI ranges between 0 and 25 with an average of 5 and a median of 4. DRG 331 shows a CCI between 0 and 25 with an average and median of 3.
Statistical analysis
Analysis of variance (ANOVA) analyses and independent t-tests were utilized to evaluate and compare group demographics and to compare the mean values of the following dependent variables: postoperative hospital LOS, RA rate within 30 and 90 days, average charge information, and rate of postoperative complications (including morbidity and mortality). Percent utilization was established by collecting the number of patients who were invoiced for at least one of the DRG codes listed above within 90 days after the surgical procedure. All statistical analyses were performed using The R Foundation© statistical software package, with statistical significance defined as P < 0.05. Top quartile and top 10th percentile were stratified for each individual DRG, with demographic, cost, and RA analysis performed for each. Statistical significance was tested between each subgroup for average cost, LOS, and comorbidity. Comorbidity was quantified by use of the CCI. Statistical regression analysis was performed using LOS, CCI, and demographics data to quantify average cost per patient. Extrapolations were then made to project cost-savings after implementation of ERPs in small community hospitals.
| Results | ▴Top |
In this retrospective study, the implementation of the ERP for bowel surgery at HCH significantly decreased LOS without increasing hospital RA rates, morbidity, or complications. When compared to national CMS data, the ERP implemented at HCH also demonstrated decreased LOS without increasing hospital RA rates, morbidity, or complications.
RA rate and LOS data between ERP and non-ERP patients at HCH
The RA rate at HCH in ERP and non-ERP cases was 3% at 30 and 90 days, without any statistical difference between the groups. The LOS was significantly reduced in the ERP group compared with the non-ERP group. This is demonstrated in Figure 1, showing average LOS among surgeons prior to ERP implementation in their patients (pre: light blue bar) and after ERP implementation (post, light blue bar). When LOS was compared by the surgeon’s average LOS among patients, compared before and after ERP implementation, LOS was significantly reduced in the ERP group after implementation of the protocol (Fig. 1a-c).
RA rate and LOS data between ERP and non-ERP patients at HCH compared to national CMS data
The RA rate at HCH in ERP and non-ERP cases was 3% at 30 and 90 days. For DRG 329, CMS has shown an RA rate of 25.1% at 90 days and 9.9% at 30 days; for DRG 330, the RA was 18.3% at 90 days and 6.6% at 30 days and DRG 331 RA was 11% at 90 days and 3.9% at 30 days.
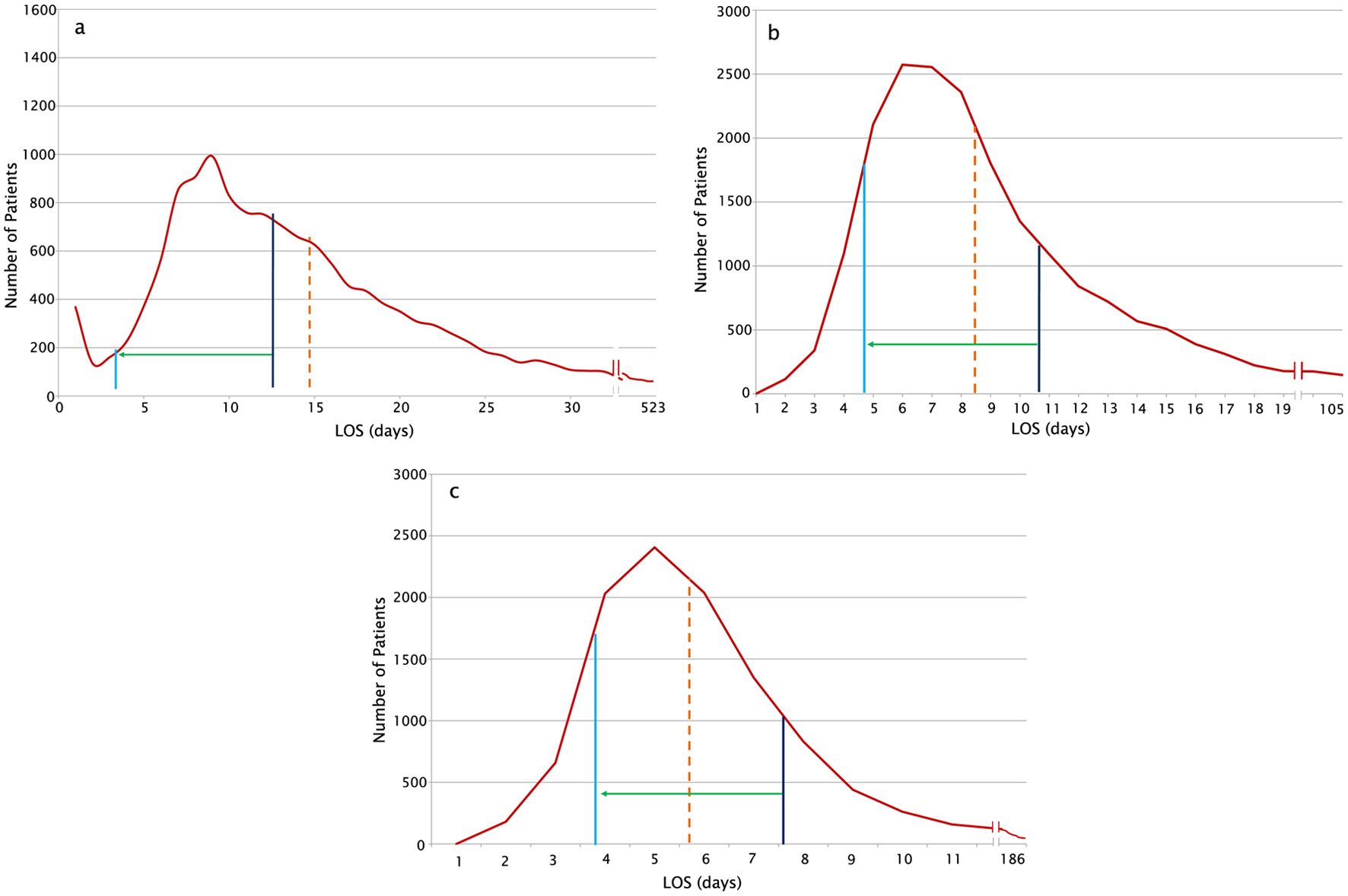
For all three DRG codes, there was a statistically significant reduction in LOS at HCH as demonstrated in Figure 2a-c. ERP at HCH improved LOS after major bowel surgery compared to Humana data. The LOS was statistically significantly reduced for all three DRG codes, as demonstrated in Figure 3a-c. In addition, when compared to other hospitals in the CMS database, the LOS at our community hospital migrated to the top percentiles for reduced LOS after bowel surgery, as demonstrated by the green arrow in Figure 4a-c, which shows the migration along a distribution curve of the average LOS after bowel surgery per DRG in the CMS database. Based on the CMS data, the migration was from the 10th percentile before ERP, to the 90th, 72nd and 54th percentile after ERP, per DRG, respectively. The improvement in LOS was achieved without any change in RAs, remaining stable at 3%, at 30 and 90 days.
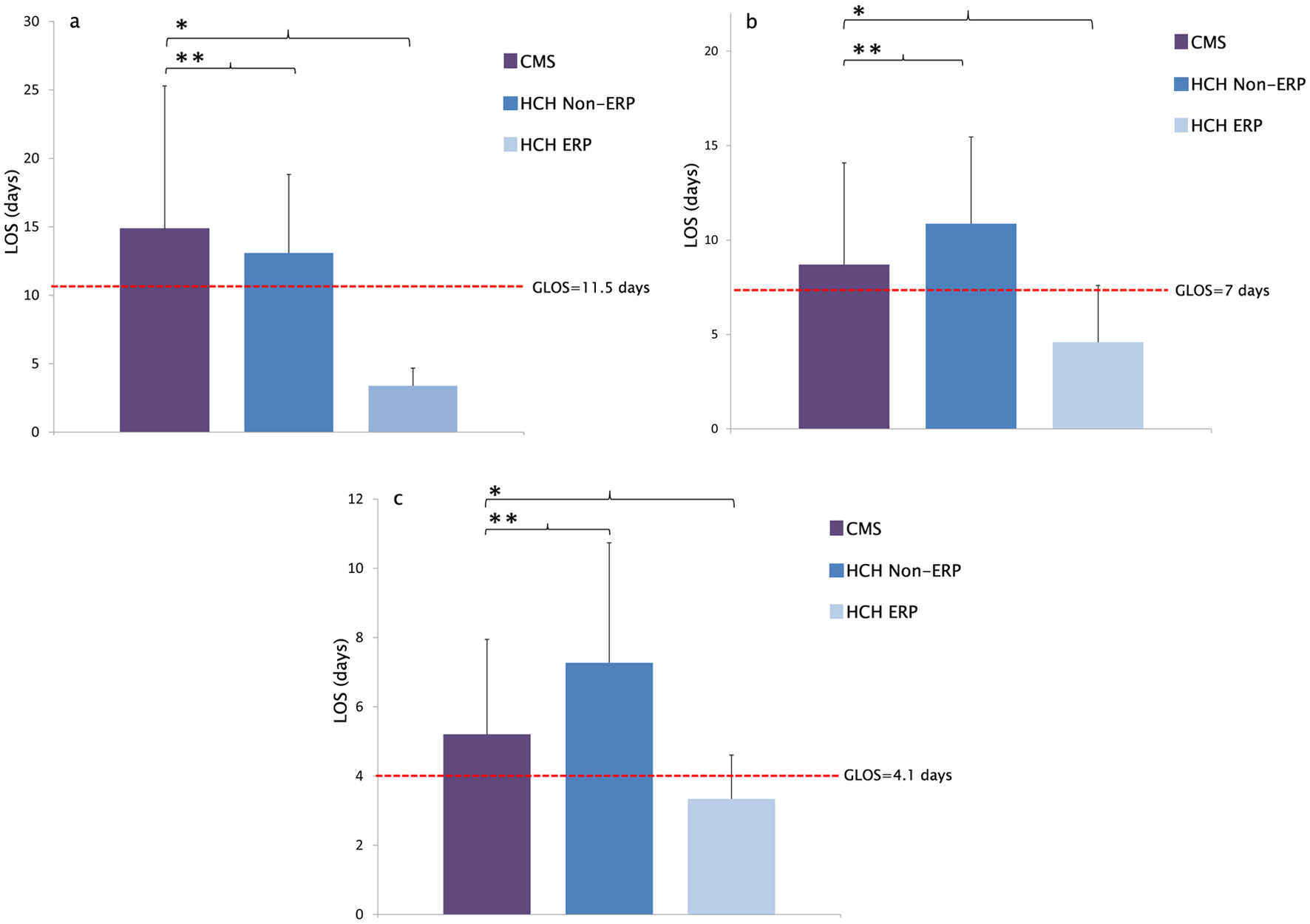 Click for large image | Figure 2. (a) CMS average LOS distribution for DRG 329 (2007 - 2012) compared with HCH. LOS significantly improved in patients undergoing ERP compared to CMS LOS (*Reduction in LOS (days) 14.870 vs. 3.375 (*P = 5.76 × 10-9). There was no significant difference in LOS between non-ERP and CMS (**Reduction in LOS (days) 14.87 vs. 13.083 (**P = 0.324)). (b) CMS average LOS distribution for DRG 330 (2007 - 2012) compared with HCH. LOS significantly improved in patients undergoing ERP compared to CMS LOS (*Reduction in LOS (days) 8.73 vs. 4.58 (*P = 2.03 × 10-6). There was no significant difference in LOS between non-ERP and CMS (**Difference in LOS (days) 8.73 vs. 10.861 (**P = 0.01)). (c) CMS average LOS distribution for DRG-331 (2007 - 2012) compared with HCH. LOS significantly improved in patients undergoing ERP compared to CMS LOS (*Reduction in LOS (days) 5.2 vs. 3.34 (*P = 0.002)). There was no significant difference in LOS between non-ERP and CMS (**Difference in LOS (days) 5.2 vs. 7.27 (**P = 0.045)). ERP: enhanced recovery protocol; DRG: diagnostic-related group; LOS: length of stay; HCH: Holy Cross Hospital. |
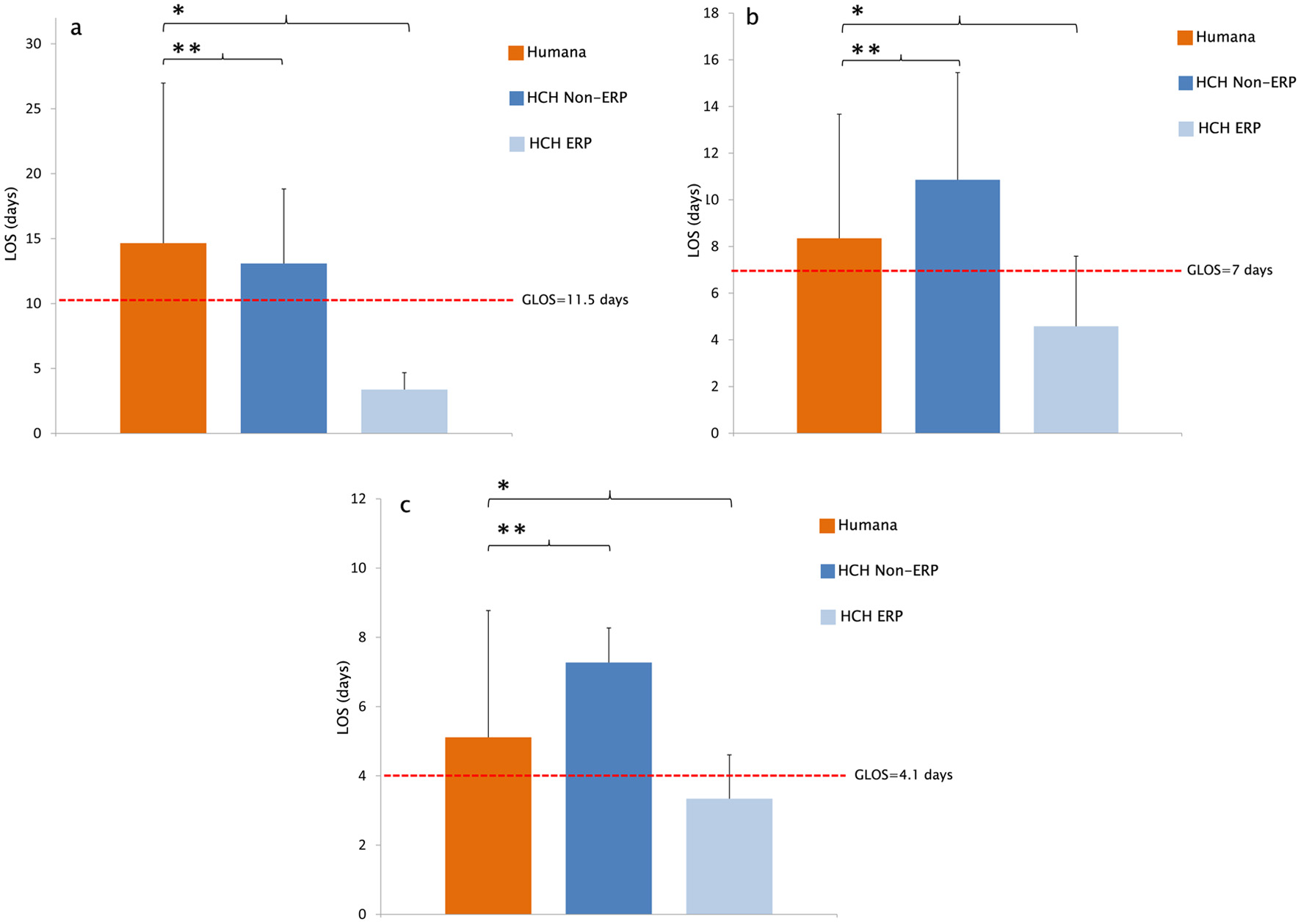 Click for large image | Figure 3. (a) Humana average LOS distribution for DRG 329 (2007 - 2015) compared with HCH. LOS significantly improved in patients undergoing ERP compared to Humana LOS (*Reduction in LOS (days) 14.65 vs. 3.375 (*P = 1.28 × 10-10)). There was no significant difference in LOS between non-ERP and Humana (**Reduction in LOS (days) 14.87 vs. 13.08 (**P = 0.354)). (b) Humana average LOS distribution for DRG 330 (2007 - 2015) compared with HCH. LOS significantly improved in patients undergoing ERP compared to Humana LOS (*Reduction in LOS (days) 8.35 vs. 4.58 (*P = 2.89 × 10-5)). There was no significant difference in LOS between non-ERP and Humana (**Difference in LOS (days) 8.35 vs. 10.86 (**P = 0.354)). (c) Humana average LOS distribution for DRG 331 (2007 - 2015) compared with HCH. LOS significantly improved in patients undergoing ERP compared to Humana LOS (*Reduction in LOS (days) 5.11 vs. 3.34 (*P = 0.0001)). There was no significant difference in LOS between non-ERP and Humana (**Difference in LOS (days) 5.11 vs. 7.27 (**P = 0.354)). ERP: enhanced recovery protocol; DRG: diagnostic-related group; LOS: length of stay; HCH: Holy Cross Hospital. |
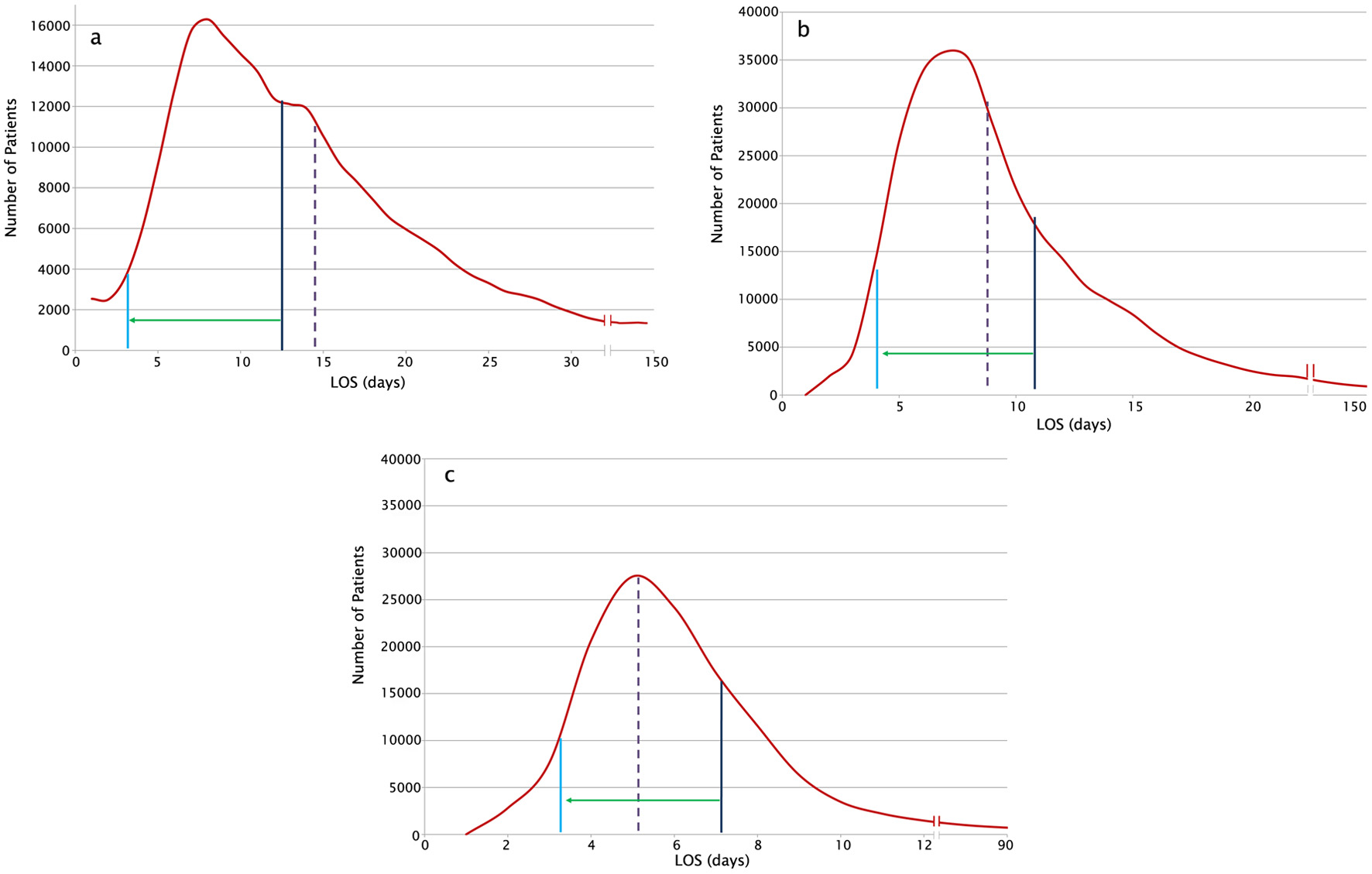 Click for large image | Figure 4. (a) The curve plots the distribution of LOS for DRG 329 at all hospitals in the CMS database. HCH non-ERP LOS is represented by the dark blue line. HCH ERP LOS is represented by the light blue line. CMS LOS is represented by the dashed purple line. The green arrow demonstrates the migration along the distribution curve, bringing HCH into the left skew after implementation of ERP. Reduction in LOS (days) 14.870 vs. 3.375 (P = 5.76 × 10-9). (b) The curve plots the distribution of LOS for DRG 330 at all hospitals in the CMS database. HCH non-ERP LOS is represented by the dark blue line. HCH ERP LOS is represented by the light blue line. CMS LOS is represented by the dashed purple line. The green arrow demonstrates the migration along the distribution curve, bringing HCH into the left skew after implementation of ERP. Reduction in LOS (days) 8.73 vs. 4.583 (P = 2.039 × 10-6). (c) The curve plots the distribution of LOS for DRG 331 at all hospitals in the CMS database. HCH non-ERP LOS is represented by the dark blue line. HCH ERP LOS is represented by the light blue line. CMS LOS is represented by the dashed purple line. The green arrow demonstrates the migration along the distribution curve, bringing HCH into the left skew after implementation of ERP. Reduction in LOS (days) 5.20 vs. 3.348 (P = 0.002). ERP: enhanced recovery protocol; DRG: diagnostic-related group; LOS: length of stay; HCH: Holy Cross Hospital. |
In addition, when compared to other hospitals in the Humana database, the LOS at our community hospital migrated to the top percentiles for reduced LOS after bowel surgery, as demonstrated by the green arrow in Figure 5a-c, which shows the migration along a distribution curve of the average LOS after bowel surgery per DRG in the Humana database. The result in days, as well as the number of patients tracked (n) are stated for each DRG: for DRG 329, the mean LOS for non-ERP was 13.0833 days (n = 12) versus 3.375 (n = 8) (P ≤ 0.001); for DRG 330, the mean LOS for non-ERP was 10.861 days (n = 36) versus 4.583 (n = 24) (P ≤ 0.001); for DRG 331, the mean LOS for non-ERP was 7.272 days (n = 11) versus 3.348 (n = 23) (P = 0.004). Based on CMS data, at HCH the query of DRG 329 shows a significant improvement from the 10th to 90th percentile (n = 238,907), DRG 330 from 72nd to 90th percentile (n = 285,423), and DRG 331 from 10th to 54th percentile (n = 126,941) (P < 0.001).
 Click for large image | Figure 5. (a) The curve plots the distribution of LOS for DRG 329 at all hospitals in the Humana database. HCH non-ERP LOS is represented by the dark blue line. HCH ERP LOS is represented by the light blue line. Humana LOS is represented by the dashed orange line. The green arrow demonstrates the migration along the distribution curve, bringing HCH into the left skew after implementation of ERP. Reduction in LOS (days) 14.65 vs. 3.37 (P = 1.28 × 10-10). (b) The curve plots the distribution of LOS for DRG 330 at all hospitals in the Humana database. HCH non-ERP LOS is represented by the dark blue line. HCH ERP LOS is represented by the light blue line. Humana LOS is represented by the dashed orange line. The green arrow demonstrates the migration along the distribution curve, bringing HCH into the left skew after implementation of ERP. Reduction in LOS (days) 8.35 vs. 4.58 (P = 2.89 × 10-5). (c) The curve plots the distribution of LOS for DRG 331 at all hospitals in the Humana database. HCH non-ERP LOS is represented by the dark blue line. HCH ERP LOS is represented by the light blue line. Humana LOS is represented by the dashed orange line. The green arrow demonstrates the migration along the distribution curve, bringing HCH into the left skew after implementation of ERP. Reduction in LOS (days) 8.35 vs. 4.58 (P = 2.89 × 10-5). ERP: enhanced recovery protocol; DRG: diagnostic-related group; LOS: length of stay; HCH: Holy Cross Hospital. |
Demographic data analysis
When demographic data were compared between ERP and non-ERP patients at HCH, there was no difference in the median age, sex, or medical comorbidities for these patients undergoing elective major bowel surgery.
| Discussion | ▴Top |
In recent years, there has been increased interest in implementing comprehensive perioperative protocols including perioperative optimization and education, perioperative goal-directed fluid management, and postoperative fast-tracking [19]. For patients undergoing elective small bowel surgeries, such ERPs are becoming the standard of care as they maintain bowel function and reduce the incidence of postoperative ileus [20]. While previous studies have demonstrated the efficacy of bowel surgery ERPs for reducing LOS, RA rates, and complications, there is little evidence regarding their success in community hospitals [21]. The implementation of an ERP in an integrated community healthcare system requires adoption of interdisciplinary change and allocation of resources, which can cause hesitation. This study demonstrated that an ERP provided significant benefit in a community healthcare system and that ERP programs could be implemented in similar settings.
In this study, an ERP for bowel surgery was successfully introduced at HCH, which was determined by a significantly decreased LOS. HCH, MGH, and 700 other US hospitals participate in a national surgical quality improvement program, which was designed to enhance the quality of surgical care by safely replacing traditional practices. The data proven model was created to improve quality of life, preparedness for surgery, postsurgical recovery, and to assist patients in regaining presurgical performance level. To achieve these measures, a multimodal and multidisciplinary approach was utilized which included perioperative, intraoperative, and postoperative interventions. The perioperative prehabilitation program was designed to adjust to each patient’s personalized treatment plan through the collaboration of physical therapists, dieticians, social workers and other necessary specialists. Multimodal analgesia involved tailoring medication adjustment and administration to individual pain levels with minimal opioid use. Postoperatively, DVT and pulmonary embolism (PE) prophylaxis were accomplished via assisted walking on the same day of surgical intervention and gastrointestinal complications were prevented by administration of adequate or supplementary nutrition, clear liquids, and chewing gum for a minimum of 30 min. This ERP also included collaboration with the spiritual care department to reduce hospitalization-related anxiety, fear, and uncertainty, as a reduction in these measures has been associated with improved surgical outcomes.
Several limitations of this study should be discussed. Primarily, the retrospective design of the study precludes a randomized design. There are also several confounding variables that have the potential to affect study outcomes, although they were mitigated to the best of our abilities. As adherence to ERPs has been studied to affect outcome measures, the implementation of a multidisciplinary team to track outcomes was implemented to monitor adherence to the ERP. All ERP patients were in compliance with the ERP perioperative program. Additionally, the results from HCH represent the results of implementation at a single institution in a community setting and therefore may not be generalizable to other hospitals or more specifically, to academic centers. The results were compared with a national database, however, to compare our findings at HCH with a large cohort and therefore increase our generalizability to a larger population. The extensive network of hospitals included in the databases utilized for this study differed in size, capacity, and staff. The significant decrease in LOS and cost of treatment at HCH compared to these databases demonstrates that this ERP was thoroughly compared to various treatment settings and conditions and subsequently, that this ERP program can be of similar success in other community hospitals. While implementation of ERP programs requires significant change from traditional methods, decreased treatment cost, improved recovery, and expected increases in patient satisfaction justify the resource allocation. Further studies comparing the cost of ERP implementation to cost savings over time in community hospitals are recommended. These types of studies can further expand upon the financial and clinical incentive for ERP programs.
Conclusion
In this retrospective study, the implementation of an ERP developed by HCH and MGH for bowel surgery was implemented at HCH and significantly decreased LOS and hospital costs without increasing hospital RA rate, morbidity, or complications. Our findings demonstrate that this ERP not only improves outcomes for bowel surgery but can also be implemented successfully in a community setting.
Acknowledgments
The authors acknowledge the support from Dr. Kenneth Tanabe, Dr. Keith Lillemoe, and Dr. Andrew Warshaw. The authors also acknowledge the support of Holy Cross Hospital, Massachusetts General Hospital, and Nova Southeastern University Dr. Kiran C. Patel College of Allopathic Medicine.
Financial Disclosure
Grant supported by Broward Community Foundation.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was exempted as this study was conducted using de-identified data.
Author Contributions
Lexi Frankel is responsible for manuscript writing, CMS and Humana database analysis, clinical data analysis, and figures. Amalia Ardeljan is responsible for data analysis and figure and table production. Diego Maurente and Manjani Divesh are responsible for data analysis and preliminary manuscript writing. Ali M. Rashid is responsible for protocol design and implementation. Kazuaki Takabe is responsible for manuscript writing, editing, and data analysis. Omar Rashid is responsible for protocol design/implementation, manuscript writing, editing, and data analysis.
Data Availability
The authors declare that data supporting the findings of this study are extracted from Humana, CMS and patient charts, and available within the article.
Abbreviations
LOS: length of stay; RA: readmission; ERP: enhanced recovery protocol; HCH: Holy Cross Hospital; DRG: diagnostic-related group; CMS: Center for Medicare System Multidisciplinary; ERAS: enhanced recovery after surgery; HIPPA: Health Insurance Portability and Accountability Act
| References | ▴Top |
- Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78(5):606-617.
doi pubmed - Melnyk M, Casey RG, Black P, Koupparis AJ. Enhanced recovery after surgery (ERAS) protocols: Time to change practice? Can Urol Assoc J. 2011;5(5):342-348.
doi pubmed - Ljungqvist O, de Boer HD, Balfour A, Fawcett WJ, Lobo DN, Nelson G, Scott MJ, et al. Opportunities and challenges for the next phase of enhanced recovery after surgery: a review. JAMA Surg. 2021;156(8):775-784.
doi pubmed - Khanijow AN, Wood LN, Xie R, Theiss LM, Hollis RH, Hardiman KM, Gunnells DJ, et al. The impact of an enhanced recovery program (ERP) on the costs of colorectal surgery. Am J Surg. 2021;222(1):186-192.
doi pubmed - Ariffin AC, Mohammad AT, Zuhdi Z, Azman A, Othman HA, Jarmin R. Enhanced Recovery after Surgery (ERAS) implementation after pancreaticoduodenectomy: interim result. Middle East Journal of Scientific Research. 2014.
doi - Coolsen MM, Bakens M, van Dam RM, Olde Damink SW, Dejong CH. Implementing an enhanced recovery program after pancreaticoduodenectomy in elderly patients: is it feasible? World J Surg. 2015;39(1):251-258.
doi pubmed - Horres CR, Adam MA, Sun Z, Thacker JK, Moon RE, Miller TE, Grant SA. Enhanced recovery protocols for colorectal surgery and postoperative renal function: a retrospective review. Perioper Med (Lond). 2017;6:13.
doi pubmed - Grant MC, Isada T, Ruzankin P, Whitman G, Lawton JS, Dodd OJ, Barodka V, et al. Results from an enhanced recovery program for cardiac surgery. J Thorac Cardiovasc Surg. 2020;159(4):1393-1402.e1397.
doi pubmed - Cortez AR, Kassam AF, Levinsky NC, Jung AD, Daly MC, Shah SA, Rafferty JF, et al. Enhanced recovery protocol improves postoperative outcomes and minimizes narcotic use following resection for colon and rectal cancer. Surg Open Sci. 2019;1(2):74-79.
doi pubmed - Wong DL, Holland A, Kocak M, Coday M, Brown C, Monroe JJ, Hinkle NM, et al. The impact of an enhanced recovery protocol in a high-risk population undergoing colon cancer surgery. Am Surg. 2022.
doi pubmed - Rona K, Choi J, Sigle G, Kidd S, Ault G, Senagore AJ. Enhanced recovery protocol: implementation at a county institution with limited resources. Am Surg. 2012;78(10):1041-1044.
doi pubmed - Poon JT, Fan JK, Lo OS, Law WL. Enhanced recovery program in laparoscopic colectomy for cancer. Int J Colorectal Dis. 2011;26(1):71-77.
doi pubmed - Hassinger TE, Mehaffey JH, Martin AN, Bauer-Nilsen K, Turrentine FE, Thiele RH, Sarosiek BM, et al. Implementation of an enhanced recovery protocol is associated with on-time initiation of adjuvant chemotherapy in colorectal cancer. Dis Colon Rectum. 2019;62(11):1305-1315.
doi pubmed - Byrne BE, Faiz OD, Bottle A, Aylin P, Vincent CA. A protocol is not enough: enhanced recovery program-based care and clinician adherence associated with shorter stay after colorectal surgery. World J Surg. 2021;45(2):347-355.
doi pubmed - Hamel JF, Sabbagh C, Alves A, Regimbeau JM, Vignaud T, Venara A. Comparison of treatment to improve gastrointestinal functions after colorectal surgery within enhanced recovery programmes: a systematic review and meta-analysis. Sci Rep. 2021;11(1):7423.
doi pubmed - Martinez-Escribano C, Arteaga Moreno F, Perez-Lopez M, Cunha-Perez C, Belenguer-Varea A, Cuesta Peredo D, Blanco Gonzalez FJ, et al. Malnutrition and increased risk of adverse outcomes in elderly patients undergoing elective colorectal cancer surgery: a case-control study nested in a cohort. Nutrients. 2022;14(1):207.
doi pubmed - Merchant SJ, Ituarte PH, Choi A, Sun V, Chao J, Lee B, Kim J. Hospital readmission following surgery for gastric cancer: frequency, timing, etiologies, and survival. J Gastrointest Surg. 2015;19(10):1769-1781.
doi pubmed - Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103(2):117-128.
doi pubmed - Nanavati AJ, Prabhakar S. Fast-track surgery: Toward comprehensive peri-operative care. Anesth Essays Res. 2014;8(2):127-133.
doi pubmed - Khawaja ZH, Gendia A, Adnan N, Ahmed J. Prevention and management of postoperative ileus: a review of current practice. Cureus. 2022;14(2):e22652.
doi - Cavallaro P, Bordeianou L. Implementation of an ERAS pathway in colorectal surgery. Clin Colon Rectal Surg. 2019;32(2):102-108.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Oncology is published by Elmer Press Inc.


