| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://www.wjon.org |
Original Article
Volume 14, Number 5, October 2023, pages 401-405
Improving Value in Colorectal Cancer Care: An Economic Analysis of Enhanced Recovery Protocols at a Community Hospital
Lexi Frankela, b, Amalia D. Ardeljana, Ali Rashida, Abhishek Nairc, Kazuaki Takabed, e, Omar M. Rashida, b, f, g, h, i, j, k, l, m
aDepartment of Surgery, Michael and Dianne Biennes Comprehensive Cancer Center, Holy Cross Health, Fort Lauderdale, FL, USA
bNova Southeastern University, Dr. Kiran C. Patel College of Allopathic Medicine, Fort Lauderdale, FL, USA
cRapides Regional Medical Center, Alexandria, LA, USA
dDepartment of Surgical Oncology, Roswell Park Comprehensive Cancer Center, Buffalo, NY, USA
eDepartment of Surgery, University at Buffalo Jacobs School of Medicine and Biomedical Sciences, The State University of New York, Buffalo, NY, USA
fUniversity of Miami, Leonard Miami School of Medicine, Miami, FL, USA
gDepartment of Surgical Oncology, Massachusetts General Hospital, Boston, MA, USA
hDepartment of Surgical Oncology, Broward Health, Fort Lauderdale, FL, USA
iTopLine MD Alliance, Fort Lauderdale, FL, USA
jDepartment of Surgical Oncology, Memorial Health, Pembroke Pines, FL, USA
kDepartment of Surgical Oncology, Delray Medical Center, Delray, FL, USA
lComplex General Surgical Oncology, General & Robotic Surgery, TopLine MD Alliance, Fort Lauderdale, FL 33308, USA
mCorresponding Author: Omar M. Rashid, Complex General Surgical Oncology, General & Robotic Surgery, TopLine MD Alliance, Fort Lauderdale, FL 33308, USA
Manuscript submitted February 24, 2023, accepted May 17, 2023, published online September 20, 2023
Short title: Economics of ERPs at a Community Hospital
doi: https://doi.org/10.14740/wjon1580
| Abstract | ▴Top |
Background: Enhanced recovery protocols (ERPs) have been shown to improve the outcomes of gastrointestinal cancer care, leading to reduced morbidity of gastrointestinal treatment and reduced delays in systemic therapy. ERP implementation has also previously shown a reduction in length of stay (LOS) without changing the readmission rate; however, the economic cost associated with these measures has not yet been quantified. The aim of this study was to evaluate the economic costs of ERP implementation for colorectal cancer at a community hospital.
Methods: The Diagnostic Related Group (DRG) codes were used to assess costs associated with the hospitalizations of cases in the ERP versus non-ERP groups. The American Hospital Association (AHA) Annual Survey from 1999 to 2015 was used to provide the expenses per day for inpatient hospitalization in the United States. Postoperative LOS, average healthcare costs, and postoperative complications between ERP-protocol and non-ERP protocol groups were analyzed using analysis of variance (ANOVA) and independent t-tests.
Results: The AHA survey estimated that $2,265 was incurred per day for non-profit hospitals in Florida and $2,346 was incurred per day for the United States. For all DRG codes, the ERP-participating group was associated with a shorter LOS and reduced health care costs. LOS-associated cost was compared between ERP and non-ERP groups: for DRG 329, the total savings was $162,118.8 (n = 12 non-ERP versus n = 8 ERP, P = 4.39 × 10-18); for DRG 330, $314,552.64 (n = 36 non-ERP versus n = 24 ERP, P = 2.72 × 10-22); and for DRG 331, $89,302.73 (n = 11 non-ERP versus n = 23 for ERP, P = 4.19 × 10-20).
Conclusions: The implementation of an ERP protocol for colorectal cancer was associated with significantly reduced costs in a community hospital.
Keywords: Expenses; Reduction; Recovery; Surgery; ERP; Length of stay; Readmission rates
| Introduction | ▴Top |
Enhanced recovery protocols (ERPs) are multidisciplinary perioperative care pathways that have been shown to improve surgical outcomes and to reduce postsurgical complications [1]. While ERPs have become the standard of care for patients undergoing elective small bowel surgeries, several hospital systems have been reluctant to adopt these protocols because they require change from traditional methods and significant resource allocation. Community hospitals in particular, which generally have less funding for research, have not implemented and studied ERP protocols as extensively as larger hospital systems [2].
ERP programs for bowel surgery have been associated with several positive surgical outcomes, including the decreased incidence of postoperative ileus and nosocomial infections, early postsurgical recovery and mobility, and decreased opioid resistance [3]. As postoperative complications are the strongest indicator of healthcare costs [4], the role of ERP programs in reducing these complications has important implications for the financial wellbeing of patients and hospitals.
While some studies have demonstrated that ERP implementation trends towards lower medical costs [5], several previous studies did not reach statistical significance, included a small sample size, or were conducted at large academic medical centers [6, 7]. There has been increased interest in the efficacy of ERP programs in community settings because several large academic facilities are attempting to merge with community hospitals to improve patient care [2]. In order to examine the financial efficacy of ERP programs in multiple clinical settings, they require implementation and evidence-based analysis in settings such as community hospitals. The aim of this study was to assess and evaluate the economic impact of ERP implementation at a community hospital.
| Materials and Methods | ▴Top |
Data sources and study population
Diagnostic Related Group (DRG) codes were used to identify 114 patients undergoing major bowel resection (DRG 329, DRG 330, DRG 331) at the Holy Cross Hospital (HCH), a small community hospital in Fort Lauderdale, Florida (Table 1). Patients were stratified into two comparison groups: ERP protocol (Table 2) (“ERP”, n = 55) and non-ERP protocol (“non-ERP”, n = 59), which received care by the same group of board-certified surgeons. The cost for length of stay (LOS) was estimated using two components: the hotel cost, which included the overhead fees associated with the hospital stay itself, and the treatment cost, which included direct costs to patients. DRG codes were used to assess costs associated with the hospitalizations of cases in the ERP versus non-ERP groups. The American Hospital Association (AHA) Annual Survey from 1999 to 2015 was used to provide the expenses per day for inpatient hospitalization in the United States. These two components (hotel cost and treatment cost) comprise the total cost for the LOS and were therefore used to estimate total average healthcare costs.
 Click to view | Table 1. Descriptions of DRG Codes Used to Identify Disease Classifications |
 Click to view | Table 2. Perioperative Interventions in ERP Versus Non-ERP Protocol |
Statistical analysis
Comparison of postoperative LOS between ERP-protocol and non-ERP protocol groups was conducted using analysis of variance (ANOVA) and independent t-tests. Average healthcare costs and postoperative complications were also analyzed using ANOVA and independent t-tests. Statistical analyses were calculated using the R Foundation© statistical software package and statistical significance was defined as P < 0.05. Charlson Comorbidity Index (CCI) was used to predict mortality based on comorbidities. Statistical regression analysis was performed using postoperative LOS, CCI, and patient demographics to quantify the average cost of treatment per patient. These calculated healthcare costs were then extrapolated to project cost-savings after implementation of ERP protocols in small community hospitals.
Ethical compliance with human study
The Institutional Review Board (IRB) approval was obtained. The study was conducted using deidentified data and in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
| Results | ▴Top |
LOS data
LOS-associated cost was compared between ERP and non-ERP groups using independent t-tests (Fig. 1): for DRG 329, the total savings was $162,118.8 (n = 12 non-ERP versus n = 8 ERP, P = 4.39 × 10-18); for DRG 330, $314,552.64 (n = 36 non-ERP versus n = 24 ERP, P = 2.72 × 10-22); and for DRG 331, $89,302.73 (n = 11 non-ERP versus n = 23 for ERP, P = 4.19 × 10-20), respectively.
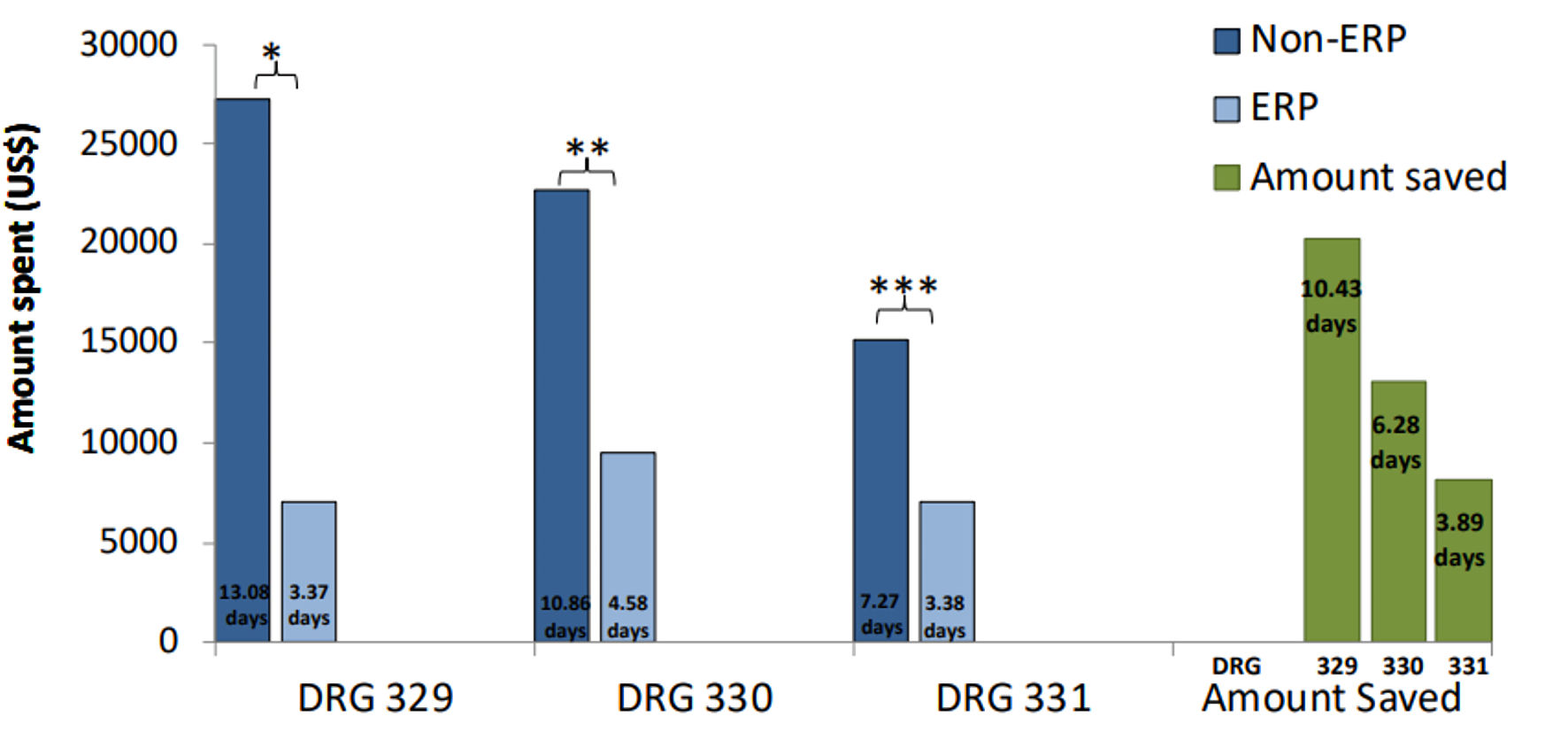 Click for large image | Figure 1. Enhanced recovery protocols showing a significant reduction in costs for each DRG code at a community hospital. X-axis is showing the Diagnostic Related Criteria; Y-axis is showing financial cost in US dollars ($) spent for a case with the corresponding average length of stay. *Reduction in costs per patient ($), P = 4.39 × 10-4. **Reduction in costs per patient ($), P = 2.72 × 10-22. ***Reduction in costs per patient ($), P = 4.19 × 10-20. ERP: enhanced recovery protocol. |
Financial data
The AHA survey estimated that $2,265 was incurred in expenses per day for non-profit hospitals in Florida and $2,346 per day for the United States. At the Holy Cross Hospital (HCH) in Fort Lauderdale, Florida, the LOS was reduced significantly in the ERP-participating group compared to the non-ERP group for each DRG code (Fig. 2). For DRG 329, the reduction in LOS at a community hospital in the ERP participating group reduced the cost of hospitalization from $27,297.96 (13.08 days) in the non-ERP participating group to $7,033.19 (3.37 days) in the ERP group. For DRG 329, ERP implementation reduced the cost by an average of $20,264.77 per patient. For DRG 330, the reduction in LOS at a community hospital in the ERP participating group reduced the cost of hospitalization from $22,664.82 (10.86 days) in the non-ERP participating group to $9,558.46 (4.58 days). For DRG 330, ERP reduced the cost by an average of $13,106.36 per patient. For DRG 331, the reduction in LOS at a community hospital in the ERP participating group reduced the cost of hospitalization from $15,172.49 (7.27 days) in the non-ERP participating group to $7,054.06 (3.38 days). For DRG 331, ERP reduced the cost by an average of $8,118.43 per patient.
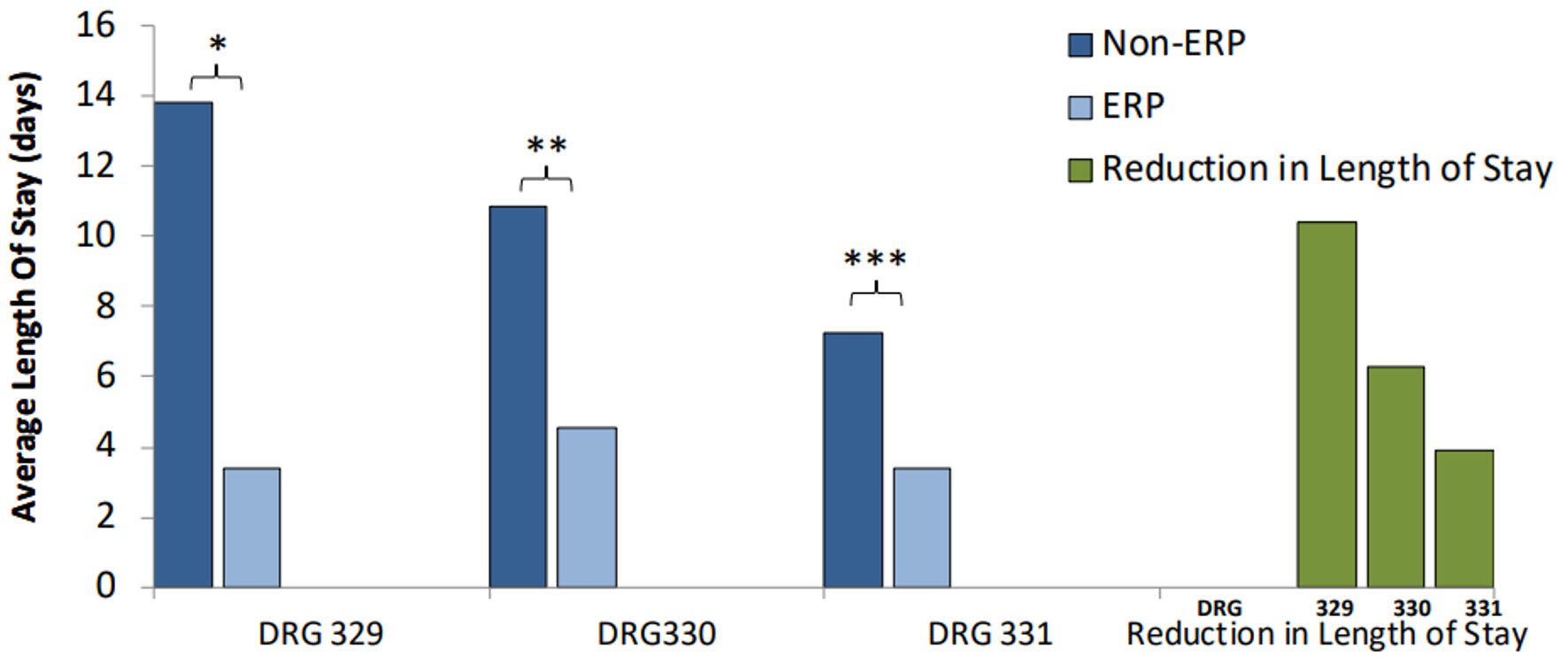 Click for large image | Figure 2. Average length of stay (LOS) is significantly reduced in patients undergoing the enhanced recovery protocols, represented by the light blue columns. Green columns are showing the number of spared hospitalization days in a patient undergoing the enhanced recovery after surgery (ERAS) protocol at a community hospital. X-axis corresponds to the Diagnostic Related Criteria (DRG) group; Y-axis is showing the LOS in days. *Reduction in LOS (days): 13.08 vs. 3.37, P = 6.99 × 10-5. **Reduction in LOS (days): 10.86 vs. 4.58, P = 1.31 × 10-7. ***Reduction in LOS (days): 7.27 vs. 3.34, P = 0.004. ERP: enhanced recovery protocol. |
| Discussion | ▴Top |
Implementing evidence-based methods to decrease surgical costs without sacrificing surgical quality has vital implications for national healthcare. The rising cost of healthcare in combination with limited community resources drives the importance of incorporating cost-effective programs that prevent resource waste. With increasing pressure from patients and insurance companies to publish and compare treatment costs and quality, studies examining ERP programs provide such comparisons and justify resource allocation. As healthcare moves towards consolidation of academic medical centers and community hospitals [2], it is more vital than ever to assure that ERPs can be successful in both settings. In this study, implementation of an ERP was not only successful in reducing costs and improving quality measures, but it also showed success in a community setting.
The presence of surgical complications is the main predictor of healthcare costs. Severe complications can lead to a five-fold increase in hospital costs compared to patients without complications. Even minor complications such as nausea and fatigue can delay discharge and have been associated with a 10% increase in healthcare costs [4]. In consideration of the increased costs associated with almost all complications, this ERP pathway was designed to prevent both minor and major complications. Measures such as fluid carbohydrate loading, deep venous thrombosis (DVT) and pulmonary embolus (PE) prophylaxis, early oral nutrition, and hypothermia prevention were implemented in order to prevent both minor and major complications in this study (Table 2). As a result, LOS and associated costs were significantly decreased for all studied surgical codes.
There has been controversy regarding whether readmission rates are higher with the use of an ERP pathway [8]. This study demonstrated that when an ERP was implemented for bowel surgery, readmission rates did not change. Several previous studies have also demonstrated that ERP pathways improve outcomes without increasing readmission rates in both colorectal [9] and non-colorectal abdominal [10] surgeries. Few studies have also demonstrated the success of ERP pathways for colorectal surgery in community settings [5, 11]. While there is literature supporting the clinical justification for implementation of ERPs, the financial justification has not been studied as thoroughly. In an effort to decrease costs for patients and hospitals, it is suggested that future studies examine the cost-effectiveness of ERPs for other surgical fields.
There are limitations to this study that should be considered. We lacked patient demographic information because of the Health Insurance Portability and Accountability Act (HIPAA) patient protections; this prevented us from assessing for any associations between demographics and cost differences. Additionally, this study was conducted at a single community hospital and the patient population and setting may not be externally valid or reflective of other hospitals. However, the scarcity of studies examining cost reductions in community settings makes this study very impactful and suggests that ERP programs for other fields could be successful in similar settings. Hospital stays associated healthcare costs generally consist of the hotel cost and the treatment cost, which can both lead to exceedingly expensive healthcare bills. The hotel cost (for services such as administration, hospital upkeep, etc.) is constant over the course of a patient’s LOS; however, the treatment cost (for laboratory testing, operating rooms, physician care, etc.) is usually highest at the beginning of the LOS and tapers off towards the end [12]. As a result, the total cost per day for the LOS is generally lower than the cost for the beginning of the stay and higher than the cost for the end of the stay. As this study utilized reductions in LOS to estimate cost savings, it is possible that our estimations for cost reduction could be slightly overestimated. However, with savings estimated at upwards of about $20,000 per patient, even slight overestimations would translate into drastic savings for patients and hospital systems.
Conclusions
This ERP program was associated with significantly decreased LOS and healthcare costs in a community setting. At a time when healthcare costs continue to increase, methods to improve surgical quality and to decrease financial responsibility have vital implications for patients and hospitals.
Acknowledgments
The authors acknowledge the support of Holy Cross Hospital and Nova Southeastern University Dr. Kiran C. Patel College of Allopathic Medicine.
Financial Disclosure
Grant support by Broward Community Foundation.
Conflict of Interest
None to declare.
Informed Consent
Not applicable because the IRB approval was obtained, and the study was conducted using deidentified data.
Author Contributions
Lexi Frankel is responsible for manuscript writing and literature review. Amalia D. Ardeljan is responsible for data analysis and figures. Ali Rashid and Abhishek Nair are responsible for preliminary manuscript writing and protocol development. Authors Kazuaki Takabe and Omar M. Rashid are responsible for manuscript writing, editing, revision, and data analysis.
Data Availability
Data are extracted from the PearlDiver national database. The data supporting the findings of this study are available from the corresponding author upon reasonable request.
- Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78(5):606-617.
doi pubmed - Fleishon HB, Itri JN, Boland GW, Duszak R, Jr. Academic medical centers and community hospitals integration: trends and strategies. J Am Coll Radiol. 2017;14(1):45-51.
doi pubmed - Manchikanti L, Helm S, 2nd, Fellows B, Janata JW, Pampati V, Grider JS, Boswell MV. Opioid epidemic in the United States. Pain Physician. 2012;15(3 Suppl):ES9-38.
pubmed - Vonlanthen R, Slankamenac K, Breitenstein S, Puhan MA, Muller MK, Hahnloser D, Hauri D, et al. The impact of complications on costs of major surgical procedures: a cost analysis of 1200 patients. Ann Surg. 2011;254(6):907-913.
doi pubmed - Geltzeiler CB, Rotramel A, Wilson C, Deng L, Whiteford MH, Frankhouse J. Prospective study of colorectal enhanced recovery after surgery in a community hospital. JAMA Surg. 2014;149(9):955-961.
doi pubmed - Wind J, Polle SW, Fung Kon Jin PH, Dejong CH, von Meyenfeldt MF, Ubbink DT, Gouma DJ, et al. Systematic review of enhanced recovery programmes in colonic surgery. Br J Surg. 2006;93(7):800-809.
doi pubmed - Delaney CP, Zutshi M, Senagore AJ, Remzi FH, Hammel J, Fazio VW. Prospective, randomized, controlled trial between a pathway of controlled rehabilitation with early ambulation and diet and traditional postoperative care after laparotomy and intestinal resection. Dis Colon Rectum. 2003;46(7):851-859.
doi pubmed - Basse L, Thorbol JE, Lossl K, Kehlet H. Colonic surgery with accelerated rehabilitation or conventional care. Dis Colon Rectum. 2004;47(3):271-277; discussion 277-278.
doi pubmed - Greco M, Capretti G, Beretta L, Gemma M, Pecorelli N, Braga M. Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg. 2014;38(6):1531-1541.
doi pubmed - Visioni A, Shah R, Gabriel E, Attwood K, Kukar M, Nurkin S. Enhanced recovery after surgery for noncolorectal surgery? A systematic review and meta-analysis of major abdominal surgery. Ann Surg. 2018;267(1):57-65.
doi - Archibald LH, Ott MJ, Gale CM, Zhang J, Peters MS, Stroud GK. Enhanced recovery after colon surgery in a community hospital system. Dis Colon Rectum. 2011;54(7):840-845.
doi pubmed - Ljungqvist O, Thanh NX, Nelson G. ERAS-Value based surgery. J Surg Oncol. 2017;116(5):608-612.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Oncology is published by Elmer Press Inc.


