| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://www.wjon.org |
Original Article
Volume 15, Number 2, April 2024, pages 239-245
Predictive Factors of Successful Double J Stent Insertion Among Advanced Cervical Cancer Patients
Syah Mirsya Warlia, b, e, Mohd. Rhiza Z. Talac, William Saputra Wijayad
aDepartment of Urology, Faculty of Medicine, Universitas Sumatera Utara Hospital - Universitas Sumatra Utara, Medan, Indonesia
bDivision of Urology, Department of Surgery, Faculty of Medicine, Universitas Sumatera Utara - Haji Adam Malik General Hospital, Medan, Indonesia
cDivision of Urogynaecology, Department of Obstetrics and Gynaecology, Faculty of Medicine, Universitas Sumatera Utara, Medan, Indonesia
dDepartment of Urology, Faculty of Medicine, Universitas Indonesia - Haji Adam Malik General Hospital, Medan, Indonesia
eCorresponding Author: Syah Mirsya Warli, Division of Urology, Department of Surgery, Faculty of Medicine, Universitas Sumatera Utara - Haji Adam Malik General Hospital, Medan, Indonesia
Manuscript submitted May 28, 2023, accepted October 16, 2023, published online March 21, 2024
Short title: Factors of DJ Stent on Cervical Cancer
doi: https://doi.org/10.14740/wjon1631
| Abstract | ▴Top |
Background: Cervical cancer remains the most lethal and prevalent cancer among women. Obstructive uropathy is a common complication of advanced cervical cancer, caused by the expanding tumor. One of the recommended treatments for this condition is the implantation of a double J (DJ) stent. However, this procedure is challenging due to the unique characteristics of the patient. The objective of this study was to identify the variables that influence the successful insertion of a DJ stent in women with advanced cervical cancer.
Methods: This retrospective study included women who attempted to have a DJ stent implanted at the General Hospital of Adam Malik in Medan, Indonesia, between January 2020 and December 2022, and were diagnosed with advanced cervical cancer. The inclusion criteria were limited to cervical cancer patients in stages III-IV, according to the International Federation of Gynecology and Obstetrics (FIGO) staging standard, who underwent an attempt at DJ stent insertion. Patients who underwent a nephrostomy and received a DJ stent were excluded from the study. The participants were divided into two groups based on the success of the DJ stent implantation. The analysis was conducted using the logistic regression test and the Chi-square test.
Results: The study included 88 patients with advanced-stage cervical cancer, of whom 45 underwent nephrostomy and 43 received a DJ stent. The analysis revealed that lower levels of hydronephrosis (odds ratio (OR): 18.203, P = 0.001), urea (OR: 4.207, P = 0.037), and creatinine (OR: 6.923, P = 0.004), higher levels of urine output (OR: 8.26, P = 0.003), and lower cervical cancer stage (OR: 4.125, P = 0.022) were all predictors of successful DJ stent insertion.
Conclusion: For women with advanced cervical cancer, lower degrees of hydronephrosis, urea, and creatinine levels, higher urine output, and lower cervical cancer stage were all predictive factors for successful DJ stent implantation.
Keywords: Cervical cancer; Double J stent; Obstructive uropathy; Nephrostomy; Predictors
| Introduction | ▴Top |
Between 2008 and 2018, cervical cancer ranked as the third or fourth most common cancer among women. In 2018, 311,000 women died from cervical cancer worldwide, at a rate of 13.1 per 100,000 females, with 80% of these deaths occurring in developing countries. In Indonesia, cervical cancer is the second most common malignancy among women, with 32,400 new cases reported in 2018. The prognosis for early-stage cervical cancer is favorable, with a 5-year survival rate of 84.5-85.9%. However, many cases of cervical cancer are diagnosed at advanced stages due to inadequate screening, cultural norms, healthcare restrictions, and insufficient health-seeking behaviors [1].
The majority of cervical cancer cases are diagnosed at advanced stages, with more than 70% of cases falling into this category. This is associated with a low likelihood of recovery and a high fatality rate. In many of these cases, providing effective treatment is challenging due to the presence of uremia caused by obstructive uropathy. This condition is caused by either external compression or the spread of cancer to the lower ureters. Patients with this condition may have large primary tumors, advanced stages of cancer, recurrent tumors, or progressive residual disease after receiving treatment [1, 2]. Urinary obstruction is a common complication in cervical cancer patients, affecting approximately 11-44% of cases. This obstruction can progress and result in renal failure and hydronephrosis, both of which have unfavorable prognoses. Patients with cervical cancer and obstructive uropathy may also experience severe complications, such as sepsis and uremia, which can exacerbate their condition and potentially lead to mortality [1]. Obstructive uropathy leading to uremia is a prevalent issue that can worsen the disease and, if left untreated, may result in loss of consciousness or death. This condition arises due to external compression, which can cause obstructions in the renal collecting system, leading to distention of the renal calyces and the onset of hydronephrosis. This condition is potentially life-threatening and requires immediate intervention to redirect urine flow away from the obstructed kidneys [3].
Urinary diversion procedures, such as percutaneous nephrostomy or double J (DJ) stenting, are the primary treatment options for obstructive uropathy caused by cancer. Although these procedures can improve the quality of life for patients with advanced cervical cancer, research suggests that they do not significantly increase survival rates. However, there are some rare complications associated with these procedures. The outcome of the procedure is influenced by several factors, including the type and degree of obstruction, renal insufficiency, grade of hydronephrosis, systemic treatment after stent implantation, and bladder invasion on cystoscopy [1, 3]. In cases of palliative care, medical options are provided, and the patient’s preferences are respected. However, additional factors must be considered when selecting a course of action, such as the setup of endoscopic equipment, anesthesia-related issues, and the potential for time extensions due to insertion failures. Despite these considerations, the high failure rate of DJ stent implantation in patients with malignant ureteral obstruction caused by advanced cervical cancer poses a significant challenge [4]. Determining the elements that affect whether women with advanced cervical cancer will have DJ stent placement successfully is the aim of this study.
| Materials and Methods | ▴Top |
Study design and patients
A retrospective study was conducted at the General Hospital of Adam Malik in Medan, Indonesia, between January 2020 and December 2022. The study focused on women with advanced cervical cancer who underwent attempted DJ stent insertion. The inclusion criteria were women with cervical cancer at stage III-IV, as determined by the International Federation of Gynecology and Obstetrics (FIGO) staging method, who underwent attempted DJ stent insertion [5]. Women who had both a DJ stent and a nephrostomy installed were excluded from the study. The subjects were divided into two groups based on the success or failure of the DJ stent insertion. The study protocol is approved by the local ethical committee (No. 536/KEPK/USU/2023). The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
Intervention
DJ stenting is a medical procedure that involves the insertion of a thin, flexible tube, known as a stent, into the ureter to treat blockages caused by tumors, stones, or other causes. While regional anesthesia is the typical choice for the procedure, general anesthesia may be used in exceptional cases. In this study, the DJ stent was inserted via ureterorenoscopy, guided by the guiding wire to pass the level of the obstruction. Subsequently, the DJ stent was inserted and left in place to enable urine to flow from the kidney to the bladder [6].
Outcome assessment and definitions
The primary outcomes were mostly obtained retrospectively through the medical records of the General Hospital of Adam Malik in Medan, Indonesia. Hydronephrosis is defined as the swelling of one or both kidneys caused by the accumulation of urine due to an obstruction or blockage in the urinary tract. The severity of hydronephrosis is graded using the system developed by the Society of Fetal Urology (SFU) [7]. Ultrasound was used to assess the affected kidney and determine the location of the obstruction. Urea and serum creatinine levels were obtained through urinalysis, and daily urine output was measured by the amount of urine collected in the subject’s catheter bag. The variables were converted to categorical data using cut-off points determined by plotting a receiver operating characteristics (ROC) curve with reference to a previous study on serum creatinine cut-off by Jaya (3.38 mg/dL) and Situmorang et al [1, 8, 9]. Cervical cancer was defined using the FIGO staging method, and the history of radiotherapy and pelvic surgery was obtained from the patient’s previous medical records [5].
Statistical analysis
Categorical data are presented as the number (%), while numerical data are displayed as the mean and standard deviation or median and interquartile range. Statistical tests, such as t-tests, Chi-square (χ2) tests, or Fisher’s exact tests, were used to compare the two groups. Cut-off values for the numerical variables, along with their sensitivity and specificity, were determined by plotting an ROC curve. Multivariate analysis was performed using logistic regression which included initial model and final model analysis.
| Results | ▴Top |
Subject characteristics
The study included 88 cervical cancer patients who underwent DJ stent placement, consisting of 43 (48.9%) patients who successfully underwent DJ stent insertion and 45 (51.1%) patients who were not able to undergo DJ stent insertion and underwent nephrostomy. The basic characteristics of the study subjects are presented in Table 1. Numerical variables were categorized using a cut-off calculation, which was determined using the ROC curve, as shown in Figure 1.
 Click to view | Table 1. Subject Characteristics |
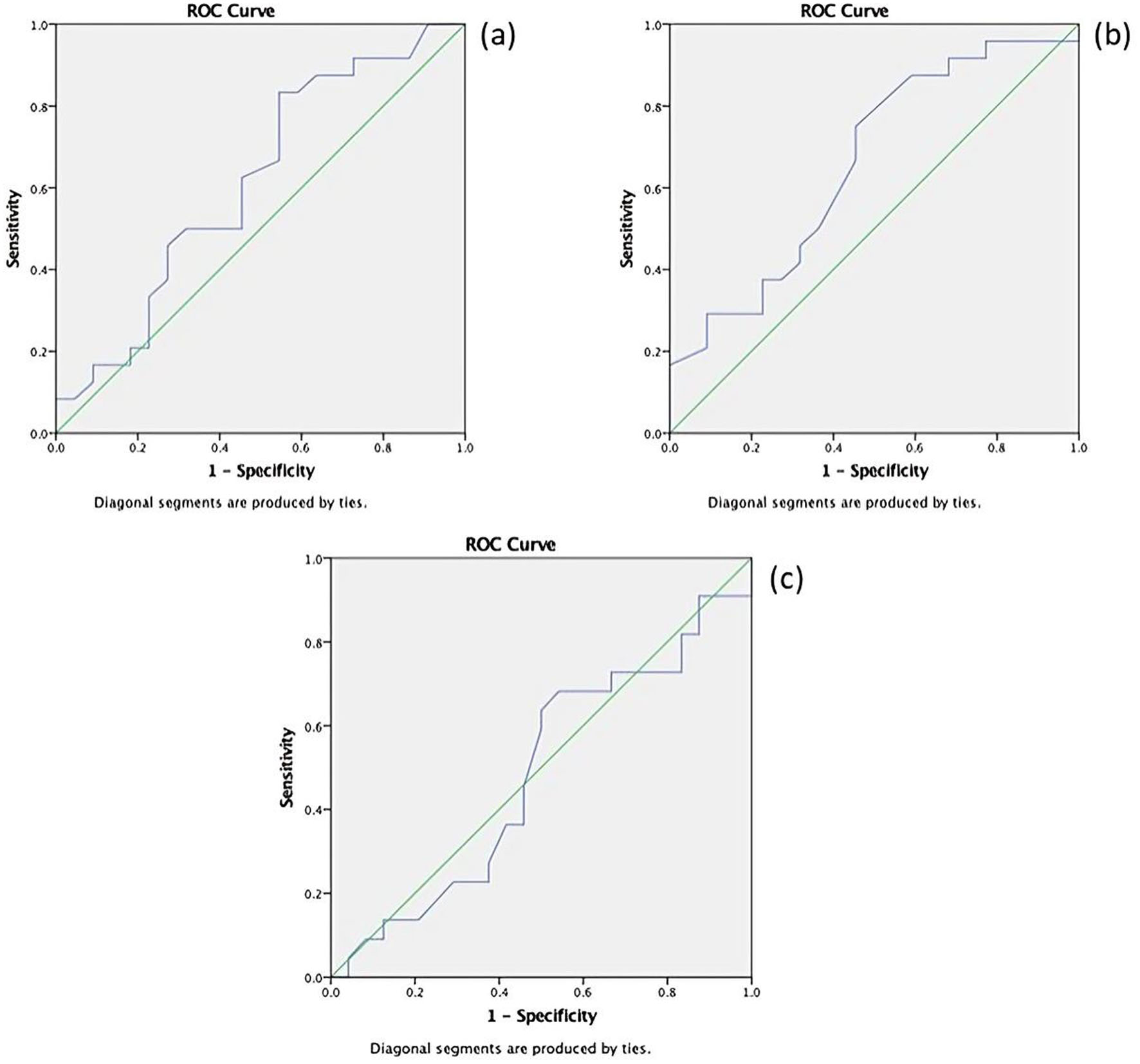 Click for large image | Figure 1. ROC curve of (a) urea, (b) creatinine, and (c) urine output. ROC: receiver operating characteristics. |
Using the values with the highest possible sensitivity and specificity, the cut-off value for urea was found to be 50 (sensitivity 87.5%, specificity 63.6%), for creatinine it was 4.0 (sensitivity 66.7%, specificity 73.3%), and for urine output it was 1,000 mL (sensitivity 64.3%, specificity 72.0%). The cut-off point for the creatinine value was consistent with a previous study conducted at Adam Malik General Hospital by Jaya [9]. In ROC curve analysis, it was shown that the area under the curve (AUC) for urea was 0.608, for creatinine was 0.716, and for urine output was 0.642. From the ROC analysis results, it was concluded that creatinine had a fair AUC value, while urea and urine output had poor AUC values. Therefore, it was inferred that creatinine had a better predictive ability compared to urea and urine output.
Bivariate analysis
After analyzing the subject characteristics, a bivariate analysis was conducted to examine the relationship between these characteristics and the success of DJ stent insertion. The relevant results are presented in Table 2.
 Click to view | Table 2. Analysis Between Subject Characteristics and Success of Insertion |
Multivariate analysis
Variables with a P-value of less than 0.25 were subjected to logistic regression analysis. The results of the analysis are presented in Table 3. The predictors of successful DJ stent insertion were found to be a lower degree of hydronephrosis (OR: 18.203, P = 0.001), lower urea level (< 50) (OR: 4.207, P = 0.037), lower creatinine level (< 4 mg/dL) (OR: 6.923, P = 0.004), higher urine output (≥ 1,000 mL) (OR: 8.26, P = 0.003), and lower cervical cancer stage (OR: 4.125, P = 0.022).
 Click to view | Table 3. Multivariate Analysis |
| Discussion | ▴Top |
Cervical cancer is a malignancy that is frequently diagnosed in women and is the fourth leading cause of mortality [1]. Compliance with screening programs is poor in developing countries, leading to the frequent diagnosis of advanced cases of cervical cancer [2]. These advanced cases can result in several complications, including anemia, sciatica, infection, and fistulas involving the bladder, rectum, and vagina. Obstructive uropathy can also develop due to decreased urine flow, causing one or both kidneys to enlarge. Gynecological cancers such as ovarian, uterine, and cervical cancer are frequent causes of obstructive uropathy in women. Concurrent radiation and cisplatin-based chemotherapy are recommended as the first line of treatment for locally advanced cervical cancer, as they can lower the risk of death and recurrence [3, 10].
Ureteral obstruction can be treated with either nephrostomy or DJ stent placement. The primary goals of treatment are to relieve symptoms, prevent complications, and assist with systemic therapy for the primary disease. Aggressive treatment is necessary while functional kidneys are available to prevent renal damage and the eventual development of uremia. Urinary diversion techniques may be considered prior to treatment to enable otherwise unfit patients to receive chemotherapy when their kidney function improves. Nephrostomy procedures are frequently performed on patients who have clinical problems or structural issues resulting from the primary illness. The choice of urine diversion method depends on the availability of equipment, the operator’s preferences, and any anesthesia-related contraindications. In cervical cancer patients with renal dysfunction due to obstructive uropathy, the decision to perform invasive nephrostomy or renal diversion should be individualized based on the availability of subsequent definitive treatment options. Nephrostomy can be an emergency temporary measure to prevent renal failure in previously treated patients with no recurrence. In carefully selected patients who present primarily with advanced disease, it can improve quality of life and prolong survival by enabling tumor-specific treatment [1-3, 10].
Currently, there is insufficient knowledge to determine the best urine diversion technique for patients with cervical cancer. Prior studies suggest that urinary diversion may improve renal function in cervical cancer patients, but its impact on overall survival rates is yet to be determined. According to Nobrega et al, treatments such as percutaneous nephrostomy and ureteral stent implantation may not provide any clinical benefits in cases of severe kidney injury and may even increase complications [3, 10].
Our research showed that DJ stent placement was successful in 43 (48.9%) out of 88 patients, while unsuccessful stent insertion resulted in the need for nephrostomy. Our results differ significantly from a similar study conducted by Affan et al, in which 69.2% of cervical cancer patients required nephrostomy [3]. Obstructive uropathy in cervical cancer can lead to the development of hydronephrosis and kidney failure, both of which have a poor prognosis. Our study showed that stent placement was unsuccessful in most patients with moderate hydronephrosis, which can result in severe complications such as sepsis and uremia, further deteriorating the patient’s condition and even leading to death [2, 10]. A study reported that hydronephrosis has prognostic value in stage IIIB cervical cancer patients. Patients with normal intravenous pyelogram and no obstruction had a 5-year survival rate of 47%, while those with ureteric obstruction without renal failure had a 5-year survival rate of 29%. Interestingly, Nobrega et al demonstrated that even after adjusting for potential confounding variables, individuals with locally advanced cervical cancer and hydronephrosis had poorer overall survival rates than those without obstructive uropathy. However, the study did not find any significant difference in progression-free survival between the two groups, and urinary diversion did not affect overall survival or progression-free survival [10].
Several studies have investigated the association between hydronephrosis and DJ stenting. Ganesarajah et al conducted a study that demonstrated the negative prognostic impact of hydronephrosis in cervical cancer patients, leading to reduced survival rates. To improve prognostication and treatment recommendations, future updates from the FIGO should consider redesignating the presence of hydronephrosis as a separate substage, specifically IIIB2. Patients with serum creatinine levels > 1.1 mg/dL or bilateral hydronephrosis should undergo treatment to relieve obstructive uropathy before initiating oncological treatment [11]. Delayed DJ stent placement can lead to severe lower urinary tract symptoms and poor renal function, resulting in a poor quality of life [12]. Patients with hydronephrosis require routine ureteral stent replacement, and depending on the stent position, they should be informed of potential consequences such as urinary infections, frank hematuria duration, back pain, and bladder spasms [13]. In a comparison of stent placement and nephrostomy, Tan et al found that while percutaneous nephrostomy may be more appropriate for individuals with more severe hydronephrosis and ureteral obstruction greater than 3 cm in length, ureteral stenting is the best treatment option for hydronephrosis secondary to cervical cancer [14].
The cervical cancer stage was found with OR 4.1 (P = 0.022) in determining success of DJ stent placement. Patients with stage IV cervical cancer have significantly poorer survival rates than those with earlier stages of the disease, and metastatic cervical cancer and performance status upon presentation are important factors in determining this rate. Lower serum creatinine levels and higher urine output were identified as positive predictors of successful DJ stent placement. While this suggests that women with lower creatinine levels may have better renal function and respond better to DJ stent insertion, it should be noted that the urea and creatinine score can be reduced by DJ stent implantation and nephrostomy, but not all patients recover renal function [1-3].
Hafsari et al conducted a meta-analysis of seven studies to evaluate the placement of DJ stents in patients with gynecological malignancies. The study found that the patient’s overall well-being should be a primary consideration when determining the appropriate treatment for ureteral obstruction and assessing the success rate of the procedure. The patient’s well-being can be evaluated through the staging of the malignancy and laboratory tests measuring kidney function. Other factors to consider include potential side effects of chemotherapy or radiotherapy and the patient’s ability to comply with stent maintenance requirements [15]. Urinary complications in cases of gynecological malignancies can significantly impact a patient’s outcomes, including graft loss, length of hospital stay, cost-effectiveness, and quality of life. Indwelling DJ ureteral stents have been widely accepted as a supplement to other urinary devices to address these complications. These stents can help relieve obstruction, prevent stenosis formation, treat urinary tract leakage, and aid in debris removal. However, the optimal duration of stent retention to reduce postoperative urinary complications remains a topic of debate. Research indicates that ureteral stents may not reduce the frequency of ureteral stricture in cervical cancer patients following radiotherapy [16, 17]. Regular stent replacement and potential complications associated with stent placement make preoperative stent placement a cautious approach in the clinical management of cervical cancer patients receiving postoperative radiotherapy [17].
The retrospective nature of the study and the lack of adequate short- and long-term follow-up limit the data and make it difficult to determine the true impact of the findings. Additionally, the study did not include other factors such as Eastern Cooperative Oncology Group (ECOG) performance status over 1, diabetes mellitus, and ascites, which can influence DJ stent placement. The study also failed to record and analyze adverse events that may occur after urinary diversions, which is important since previous reports indicate that a significant percentage of patients may experience complications such as pyelonephritis, sepsis, and severe hematuria. Patients with malignant ureteral blockage or ureteral stricture resulting from cancer treatment may require ureteral stenting. While ureteral stricture can develop into a persistent medical issue in cancer survivorship, malignant blockage has a median survival of just 3 - 6 months [1, 18].
Conclusion
Several factors, including the degree of hydronephrosis, serum urea level, serum creatinine level, urine output, and cervical cancer stage, influence the success of DJ stent insertion in advanced cervical cancer patients. Future research should record and analyze long-term follow-up and adverse events post-urinary diversions to determine their impact. Understanding the predictors of successful DJ stent insertion can help clinicians make informed decisions and improve outcomes for advanced cervical cancer patients.
Acknowledgments
The authors would like to thank Adam Malik Hospital for the support on this study.
Financial Disclosure
The authors declare no financial support or grants in the making of this study.
Conflict of Interest
The authors declare no conflict of interest in the making of this manuscript.
Informed Consent
Not applicable.
Author Contributions
Conceptualization: MSW and MRT; methodology: MSW and WSW; formal analysis and investigation: MSW; writing - original draft preparation: MSW and WSW; writing - review and editing: MSW and MRT; supervision: MRT.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Noegroho BS, Kurniawan AP, Wijayanti Z, Mustafa A. Factors affecting survival outcome after percutaneous nephrostomy as palliative urinary diversion in obstructive uropathy due to advance cervical cancer patients. Asian Pac J Cancer Prev. 2021;22(4):1211-1216.
doi pubmed pmc - Mishra K, Desai A, Patel S, Mankad M, Dave K. Role of percutaneous nephrostomy in advanced cervical carcinoma with obstructive uropathy: a case series. Indian J Palliat Care. 2009;15(1):37-40.
doi pubmed pmc - Affan MIF, Rahardjo HE, Widia F. Gynecological malignancy with obstructive uropathy patient profile in Cipto Mangunkusumo Hospital: Our 2-year experience. Bali Med J. 2022;10.
doi - Santosa KB, Prawira MM, Pramana IBP, et al. Predictor of successful DJ stent insertion in advanced cervical cancer. Open Access Maced J Med Sci. 2020;8:882-886.
doi - Salib MY, Russell JHB, Stewart VR, Sudderuddin SA, Barwick TD, Rockall AG, Bharwani N. 2018 FIGO staging classification for cervical cancer: added benefits of imaging. Radiographics. 2020;40(6):1807-1822.
doi pubmed - Das JK, Rangad GM. A new and easy technique of double-J stenting after retroperitoneal laparoscopic ureterolithotomy: A discussion of other techniques. Urol Ann. 2020;12(4):309-313.
doi pubmed pmc - Onen A. Grading of hydronephrosis: an ongoing challenge. Front Pediatr. 2020;8:458.
doi pubmed pmc - Situmorang PR, Kaban PB, Napitulu DS. Analysis of creatinine levels in failed patients chronic kidney pre and post hemodialization at Santa Elisabeth. EduHealth. 2022;13:457-459.
- Jaya E. Faktor yang mempengaruhi kegagalan pemasangan double J stent pada kanker servik. Universitas Indonesia. 2016.
- Nobrega L, Zanon JR, Andrade C, Schmidt RL, Dos Santos MH, Dos Reis R. Prognostic role of hydronephrosis in the treatment of patients with locally advanced cervical cancer: a retrospective cohort. Int J Gynecol Cancer. 2022;32(9):1123-1128.
doi pubmed pmc - Ganesarajah S, Jayapaul VC, Madhavan R, Krishnan V. The prognostic significance of hydronephrosis and role of ureteric stenting in cervical cancer patients treated with radical radiation therapy, real world outcomes from a Regional Cancer Centre, South India. Asian Pacific J Cancer Care. 2022;7:279-284.
doi - Dinatha GNK, Oka AAG, Santosa KB. Predictive factors influencing the outcomes of double “J” stent placement in stage IIIB cervical cancer patients with hydronephrosis complication. JBN (Jurnal Bedah Nasional). 2022;6:1.
doi - Li J, Cao H, Peng K, Chen R, Sun X. Hydronephrosis in patients with cervical cancer: An improved stent-change therapy for ureteral obstruction Stent-change for ureteral obstruction in cervical cancer. Eur J Obstet Gynecol Reprod Biol. 2023;283:49-53.
doi pubmed - Tan S, Tao Z, Bian X, Zhao Y, Wang N, Chen X, Wu B. Ureteral stent placement and percutaneous nephrostomy in the management of hydronephrosis secondary to cervical cancer. Eur J Obstet Gynecol Reprod Biol. 2019;241:99-103.
doi pubmed - Hafsari SR, Wardaya SAT. Success rate on double-J stenting on gynecological cancer patients: a meta-analysis study. Biosci Med J Biomed Transl Res. 2021;5:1087-1094.
doi - Liu T, Yao Y, Xing X, Chu D. Effects of continuous catheterization on reducing postoperative urinary tract infection in cervical cancer patients with Double J stent placement. J Healthc Eng. 2021;2021:9299001.
doi pubmed pmc - Liu L, Yu C, Sun F, Yang T, Wei D, Wang G, Li S, et al. Can preoperative ureteral stents reduce the incidence of ureteral stricture after radiotherapy in patients with cervical cancer? BMC Urol. 2022;22(1):106.
doi pubmed pmc - Goldfarb RA, Fan Y, Jarosek S, Elliott SP. The burden of chronic ureteral stenting in cervical cancer survivors. Int Braz J Urol. 2017;43(1):104-111.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Oncology is published by Elmer Press Inc.


