| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://www.wjon.org |
Original Article
Volume 15, Number 2, April 2024, pages 309-318
Role of Postoperative Radiotherapy on High-Risk Stage pIIIA-N2 Non-Small Cell Lung Cancer Patients After Complete Resection and Adjuvant Chemotherapy: A Retrospective Cohort Study
Zu Yi Chena, Huan Wei Liangb, Yang Liub, Wei Huangb, Xin Bin Panb, c
aDepartment of Interventional Radiology, Guangxi Medical University Cancer Hospital, Nanning, Guangxi 530021, China
bDepartment of Radiation Oncology, Guangxi Medical University Cancer Hospital, Nanning, Guangxi 530021, China
cCorresponding Author: Xin Bin Pan, Department of Radiation Oncology, Guangxi Medical University Cancer Hospital, Nanning, Guangxi 530021, China
Manuscript submitted January 30, 2024, accepted February 27, 2024, published online March 21, 2024
Short title: Postoperative Radiotherapy on pIIIA-N2 NSCLC Patients
doi: https://doi.org/10.14740/wjon1832
| Abstract | ▴Top |
Background: The aim of the study was to assess the effectiveness of postoperative radiotherapy in high-risk patients with stage pIIIA-N2 non-small cell lung cancer (NSCLC) following complete resection and adjuvant chemotherapy.
Methods: Data from NSCLC patients within the Surveillance, Epidemiology, and End Results (SEER) database were analyzed. The study examined the association between lymph node ratio (LNR) and both cancer-specific survival (CSS) and overall survival (OS) using restricted cubic spline curves. Patients were categorized into high- and low-risk groups based on established LNR cut-off values, and survival outcomes were compared between those receiving postoperative radiotherapy and those who did not within the high-risk group.
Results: The study included 1,690 patients. An LNR threshold of 0.29 was identified for both CSS and OS. Patients with an LNR ≥ 0.29 demonstrated significantly worse CSS (hazard ratio (HR) = 1.56, 95% confidence interval (CI): 1.37 - 1.78; P < 0.001) and OS (HR = 1.44, 95% CI: 1.28 - 1.62; P < 0.001) compared to those with an LNR < 0.29. In the high-risk group (LNR ≥ 0.29), postoperative radiotherapy did not significantly affect CSS (HR = 0.98, 95% CI: 0.82 - 1.17; P = 0.809) or OS (HR = 0.95, 95% CI: 0.81 - 1.11; P = 0.533).
Conclusions: LNR is a significant prognostic factor in patients with stage pIIIA-N2 NSCLC post complete resection and adjuvant chemotherapy. A higher LNR (≥ 0.29) is associated with poorer CSS and OS. However, postoperative radiotherapy does not confer survival benefits in these high-risk patients. Our findings suggest that postoperative radiotherapy should not be routinely performed in this subgroup. Further research is required to explore effective treatment strategies for these patients.
Keywords: Non-small cell lung cancer; Stage pIIIA-N2; Lymph node ratio; Postoperative radiotherapy
| Introduction | ▴Top |
Lung cancer remains the leading cause of cancer-related mortality globally, representing approximately 18% of all cancer deaths [1]. Non-small cell lung cancer (NSCLC), which accounts for about 85% of lung cancer cases, is frequently diagnosed at an advanced stage. Notably, a third of patients present with stage III disease [2]. For stage IIIA NSCLC patients, surgery-based multimodal therapies are the cornerstone of treatment [3], with adjuvant chemotherapy demonstrating improvements in both disease-free survival (DFS) and overall survival (OS) in those with completely resected pIIIA-N2 NSCLC [4-6]. However, the role of postoperative radiotherapy in this context is contentious, as reflected by varying findings in the literature [7-10].
Additionally, adjuvant epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors have been shown to further enhance DFS in patients with EGFR mutations following complete resection and adjuvant chemotherapy [11, 12]. In contrast, adjuvant immunotherapy is recommended for patients with EGFR wild-type tumors [13, 14]. While these adjuvant therapies have been associated with improved survival, various factors may influence their efficacy [15-19]. Consequently, the contribution of postoperative radiotherapy in enhancing DFS and OS in this patient population warrants further exploration.
Historically, pIIIA-N2 NSCLC was treated as a homogenous group in research. However, recent studies highlight its heterogeneity [20], which correlates with variable treatment responses [21-26]. This diversity emphasizes the importance of identifying prognostic factors to effectively stratify high-risk patients. Recommendations for postoperative radiotherapy often depend on specific risk factors, such as nodal extracapsular extension, involvement of the highest lymph node station, number of dissected mediastinal lymph node stations, number of positive mediastinal lymph node stations, and surgical approach [27, 28].
Among these factors, the prognostic significance of examined lymph nodes is an active area of research. Several studies suggest a correlation between the number of examined lymph nodes and patient survival, with higher counts linked to better outcomes [29, 30]. However, the prognostic value of lymph node examination can be influenced by the quality of the surgical procedure [31]. The lymph node ratio (LNR) (the ratio of pathologically metastatic lymph nodes to the total number of harvested lymph nodes) has emerged as a crucial prognostic factor [32-34].
This study aimed to evaluate the impact of LNR on survival outcomes in patients with pIIIA-N2 NSCLC following complete resection and adjuvant chemotherapy. It also seeks to identify high-risk patients based on their LNR and explore the potential role of postoperative radiotherapy in this subset. Our findings are intended to guide clinicians in formulating tailored treatment strategies.
| Materials and Methods | ▴Top |
Data sources
Our study utilized data from the Surveillance, Epidemiology, and End Results (SEER) program, managed by the National Cancer Institute. As a comprehensive source, SEER offers extensive data on cancer incidence, mortality, and prevalence across the United States. Data extraction was performed using SEER*Stat software (version 8.4.2), focusing on NSCLC cases from 2000 to 2020 to ensure a substantial analytical timeframe.
Study population
The study encompassed patients with histologically confirmed stage pIIIA-N2 squamous cell carcinoma and adenocarcinoma of the lung. Inclusion criteria were limited to patients who underwent radical resection and subsequent adjuvant chemotherapy. We excluded cases involving preoperative radiotherapy, segmentectomy, prior malignancies, neoadjuvant chemotherapy, or indeterminate lymph node status. Comprehensive documentation included demographic factors (age, sex, race), tumor characteristics (primary site, location, grade, histology, T stage), and lymph node status.
Endpoints
The primary endpoint was OS, which was defined as the duration from diagnosis to death from any cause. The secondary endpoint, cancer-specific survival (CSS), was the period from diagnosis to death attributable to NSCLC, as recorded in SEER data.
Stratification of lymph node ratio
In our study, the LNR was defined using the formula: LNR = PLN/TLN, where PLN represents the number of positive lymph nodes, and TLN denotes the total number of harvested lymph nodes. We investigated the prognostic significance of LNR [32-34]. Optimal cut-off values for LNR were established using restricted cubic spline methods [35-37]. This approach allowed us to explore the associations between varying LNR and key survival outcomes (CSS and OS) on a continuous scale. These associations were examined through multivariable Cox regression models, thoughtfully adjusted for a comprehensive set of confounding variables, including age, sex, race, primary site, tumor location, grade, histology, and T stage.
Statistical analysis
Age was categorized based on its median value. We compared categorical factors, including age, sex, race, primary site, tumor location, grade, histology, and T stage, across different LNR groups. These comparisons utilized the χ2 test or Fisher’s exact test, depending on the data distribution.
CSS and OS were compared between the LNR groups using Kaplan-Meier methods, followed by log-rank tests to determine statistical significance in survival differences. Independent prognostic factors impacting CSS and OS were identified using multivariable Cox regression analysis. This analysis adjusted for all the aforementioned categorical factors along with LNR group classification.
Patients were stratified into high-risk and low-risk groups based on CSS and OS outcomes in relation to LNR. High-risk patients were further categorized based on receipt of postoperative radiotherapy. We employed the χ2 test or Fisher’s exact test for comparing categorical factors between the radiotherapy and non-radiotherapy groups. Kaplan-Meier methods with log-rank tests were used to compare CSS and OS between patients who received postoperative radiotherapy and those who did not. A subsequent multivariable Cox regression analysis was conducted, incorporating radiotherapy status as a variable to identify independent prognostic factors.
Statistical analyses were conducted using SPSS Statistics Version 26.0 (IBM Co., Armonk, NY, USA) and R software (version 4.2.2). A two-tailed P value of less than 0.05 was set as the threshold for statistical significance.
Ethics approval and consent to participate
This research has obtained the Institutional Review Board approval. Ethics approval was waived by the Ethics Committee/IRB of Guangxi Medical University Cancer Hospital.
| Results | ▴Top |
Patient selection
From an initial pool of 1,007,088 lung cancer cases in the SEER database, 1,690 individuals with stage pIIIA-N2 NSCLC met our inclusion criteria. The selection process is depicted in Figure 1.
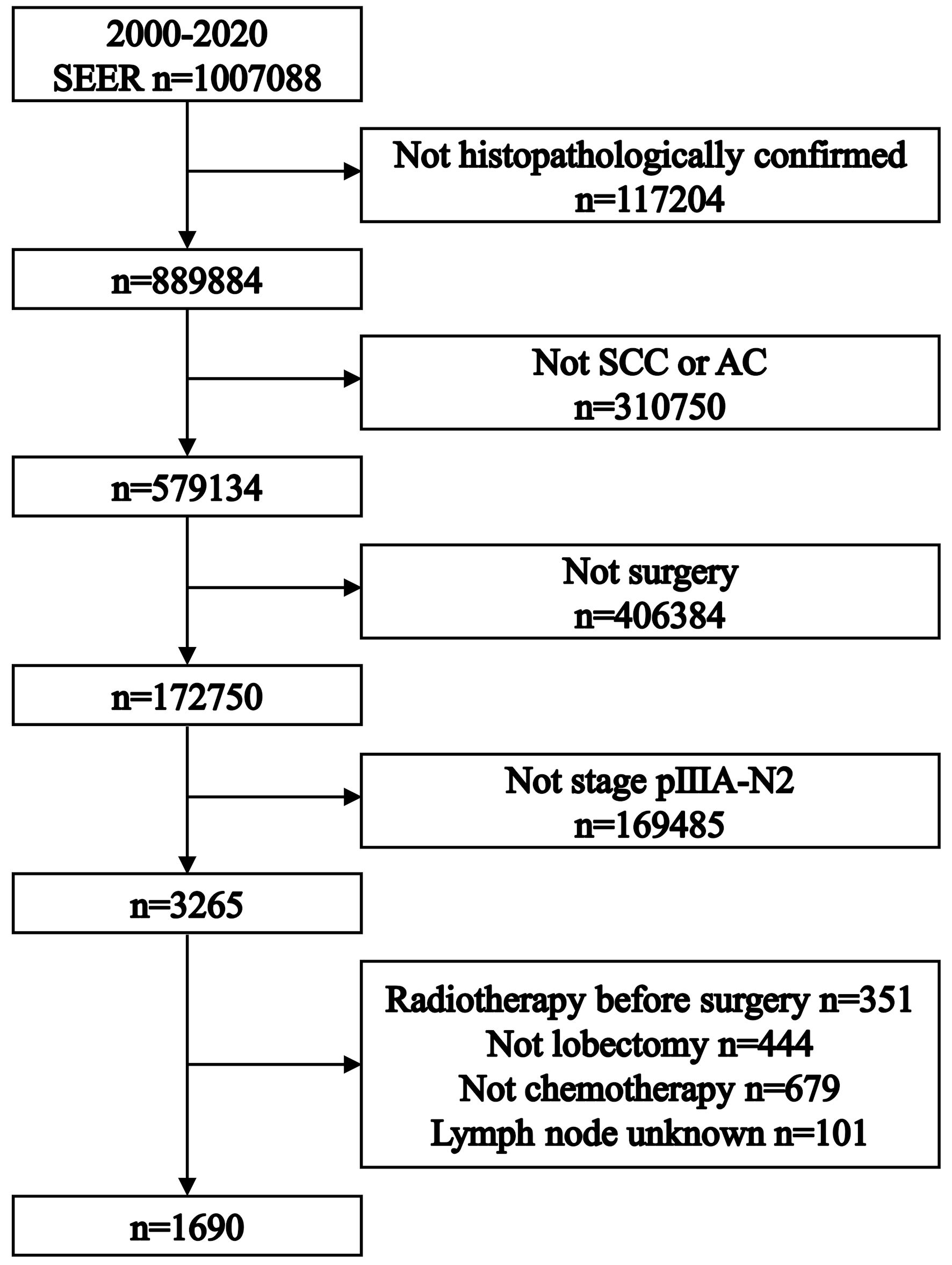 Click for large image | Figure 1. Flowchart illustrating the patient selection process for the study, outlining the criteria for inclusion and exclusion from the Surveillance, Epidemiology, and End Results database. SCC: squamous cell carcinoma. AC: adenocarcinoma. |
Association between LNR and survival outcomes
A clear relationship was observed between LNR and survival outcomes using restricted cubic spline regression, adjusted for confounding factors. The multivariable adjusted hazard ratio (aHR) is depicted by a solid red line, with the 95% confidence interval (CI) represented by the red shaded area with four knots. A horizontal solid blue line at an aHR of 1.0 serves as the reference for no association. The vertical solid blue line indicates the cut-off value. An LNR cut-off of 0.29 was identified for both CSS (Fig. 2a) and OS (Fig. 2b). Higher LNRs were linked to poorer CSS and OS.
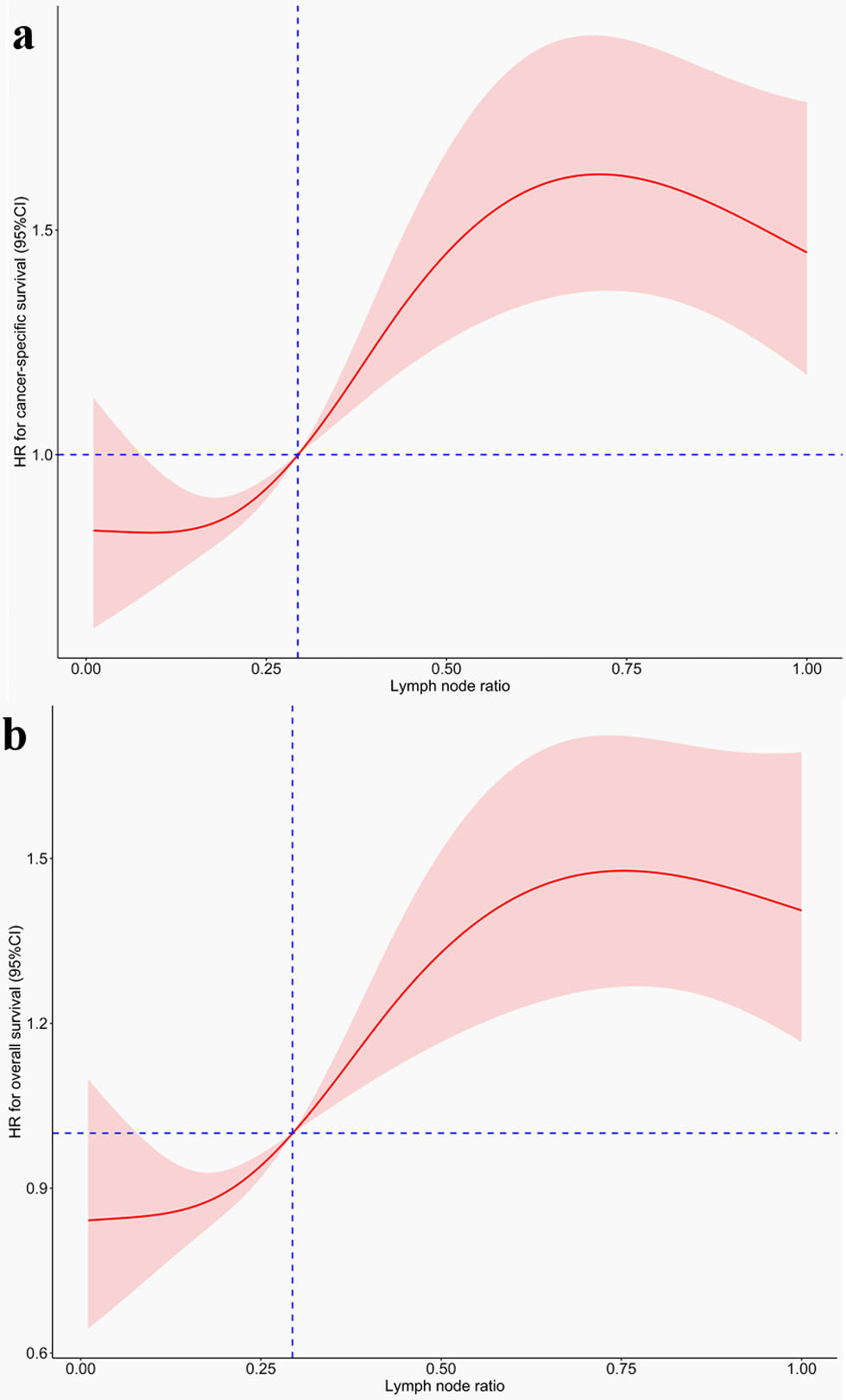 Click for large image | Figure 2. Graphs showing the association between lymph node ratio and survival outcomes, which are analyzed using restricted cubic spline regression models. (a) Cancer-specific survival. (b) Overall survival. HR: hazard ratio; CI: confidence interval. |
LNR was categorized into two categories (< 0.29 and ≥ 0.29). Baseline clinical characteristics of the two groups are summarized in Table 1.
 Click to view | Table 1. Patient Characteristics Between Different Lymph Node Ratio Groups |
Treatment outcomes across LNR groups
Patients with an LNR < 0.29 had a significantly longer median CSS of 93 months, compared to 48 months in the LNR ≥ 0.29 group (Fig. 3a). The 5-year CSS rates were 59.2% for the LNR < 0.29 group and 45.4% for the LNR ≥ 0.29 group. LNR ≥ 0.29 group was associated with decreased CSS (HR = 1.56, 95% CI: 1.37 - 1.78; P < 0.001). LNR ≥ 0.29 was independently prognostic in multivariable analysis (aHR = 1.61, 95% CI: 1.41 - 1.83; P < 0.001) (Fig. 4a).
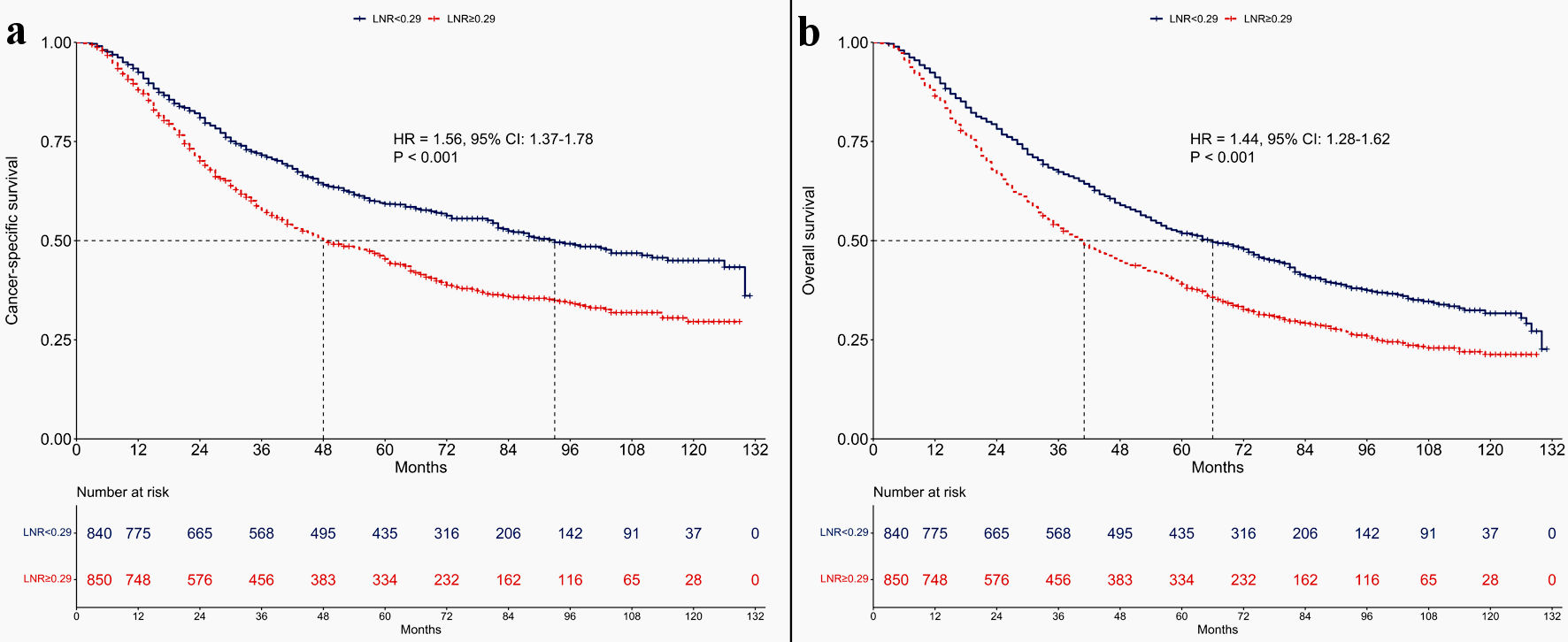 Click for large image | Figure 3. Kaplan-Meier survival curves comparing cancer-specific survival and overall survival between patients categorized by lymph node ratio: those with lymph node ratio < 0.29 versus lymph node ratio ≥ 0.29. (a) Cancer-specific survival. (b) Data on overall survival. LNR: lymph node ratio; HR: hazard ratio; CI: confidence interval. |
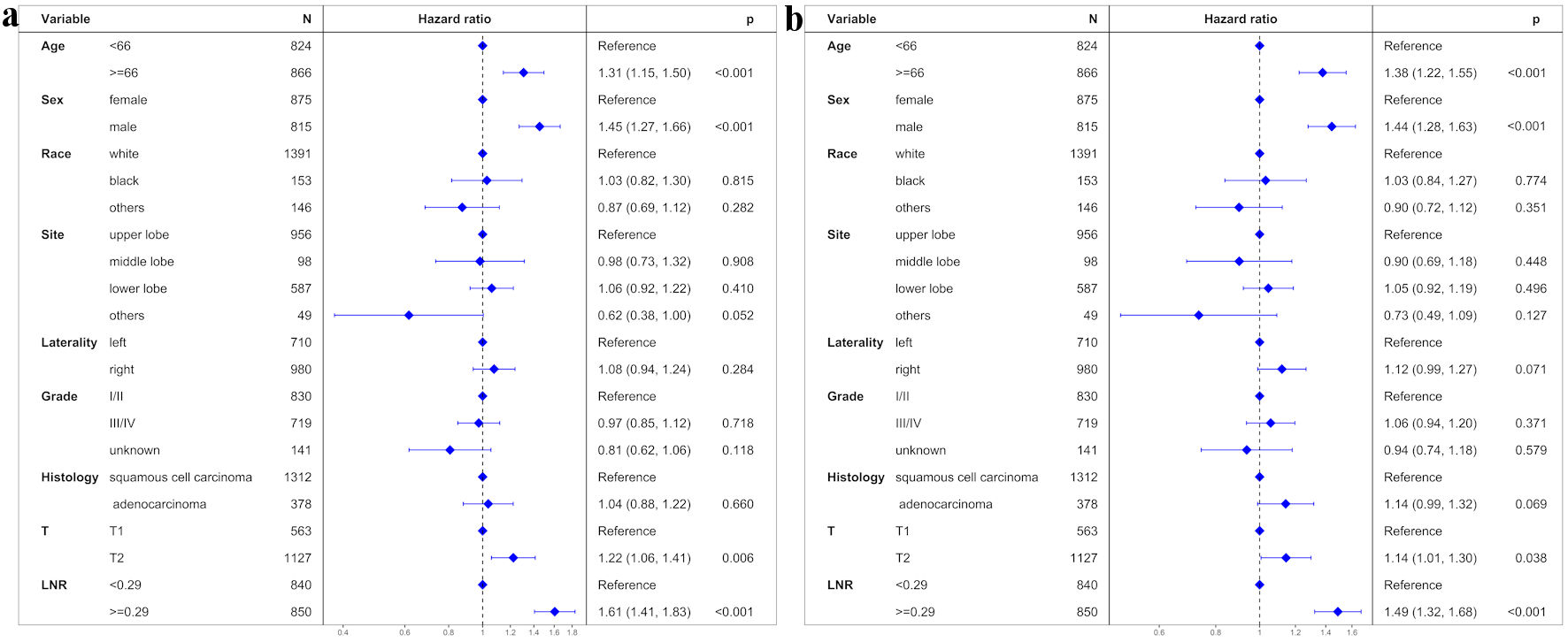 Click for large image | Figure 4. Results of multivariate regression analysis assessing various prognostic factors impacting treatment outcomes. (a) Cancer-specific survival. (b) Overall survival. LNR: lymph node ratio. |
Similarly, the median OS for patients with an LNR < 0.29 was significantly longer at 66 months, compared to 41 months for the LNR ≥ 0.29 group (Fig. 3b). The 5-year OS rates were 51.8% in the LNR < 0.29 group and 39.1% in the LNR ≥ 0.29 group. The LNR ≥ 0.29 group showed a lower OS (HR = 1.44, 95% CI: 1.28 - 1.62; P < 0.001). LNR ≥ 0.29 was independently prognostic for poorer OS (aHR = 1.49; 95% CI: 1.32 - 1.68; P < 0.001) (Fig. 4b).
Subgroup analysis in LNR ≥ 0.29 group
Patients with an LNR ≥ 0.29 were further divided into postoperative radiotherapy and non-radiotherapy groups, with baseline characteristics detailed in Table 2.
 Click to view | Table 2. Patient Characteristics Between Non-Radiotherapy and Radiotherapy Groups in Patients With Lymph Node Ratio ≥ 0.29 |
Role of postoperative radiotherapy in LNR ≥ 0.29 group
No significant differences were observed in CSS between the non-radiotherapy and radiotherapy subgroups. CSS was 47 months in the non-radiotherapy group and 49 months in the radiotherapy group. The 5-year CSS rates were 44.5% for the non-radiotherapy group and 46.1% for the radiotherapy group (HR = 0.98; 95% CI: 0.82 - 1.17; P = 0.809) (Fig. 5a). Multivariable Cox regression analysis reaffirmed no significant independent impact of radiotherapy on CSS (aHR = 0.98, 95% CI: 0.82 - 1.17; P = 0.803) (Fig. 6a).
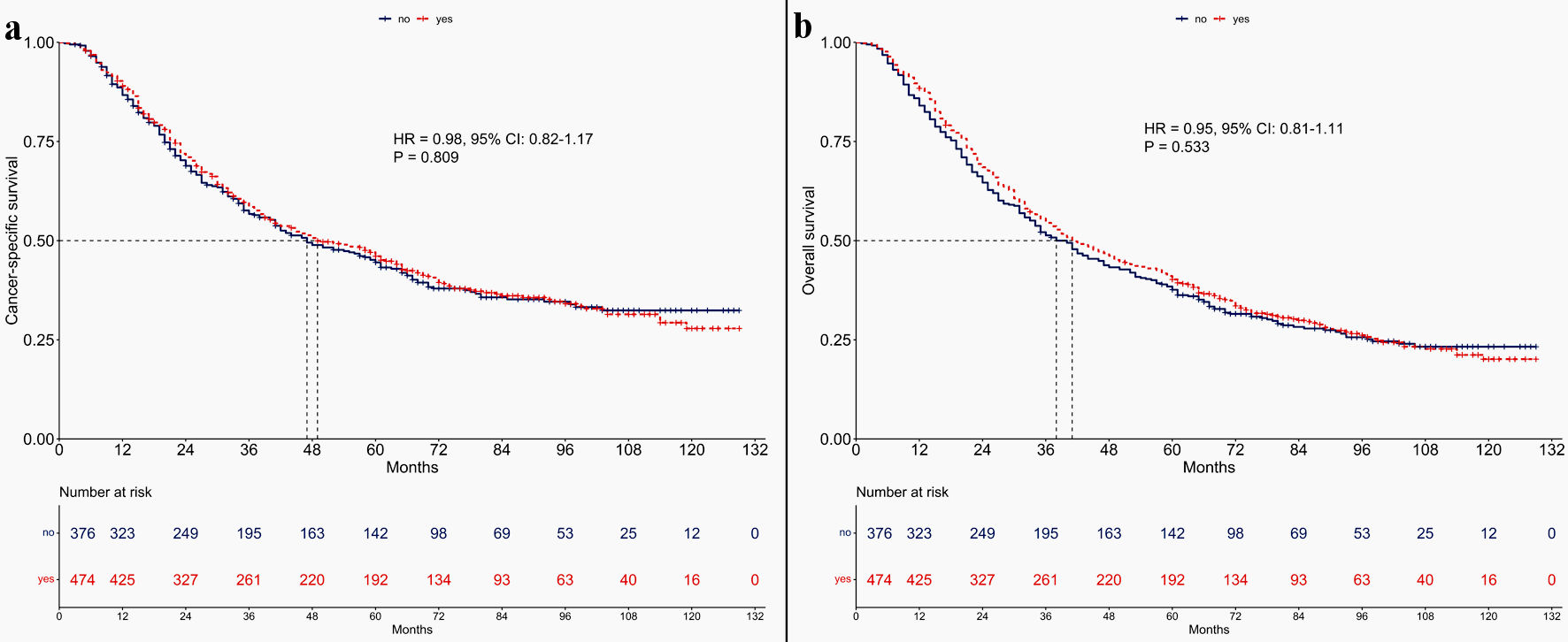 Click for large image | Figure 5. Kaplan-Meier survival curves depicting treatment outcomes between non-radiotherapy and radiotherapy groups in patients with lymph node ratio ≥ 0.29. (a) Cancer-specific survival. (b) Overall survival. HR: hazard ratio; CI: confidence interval. |
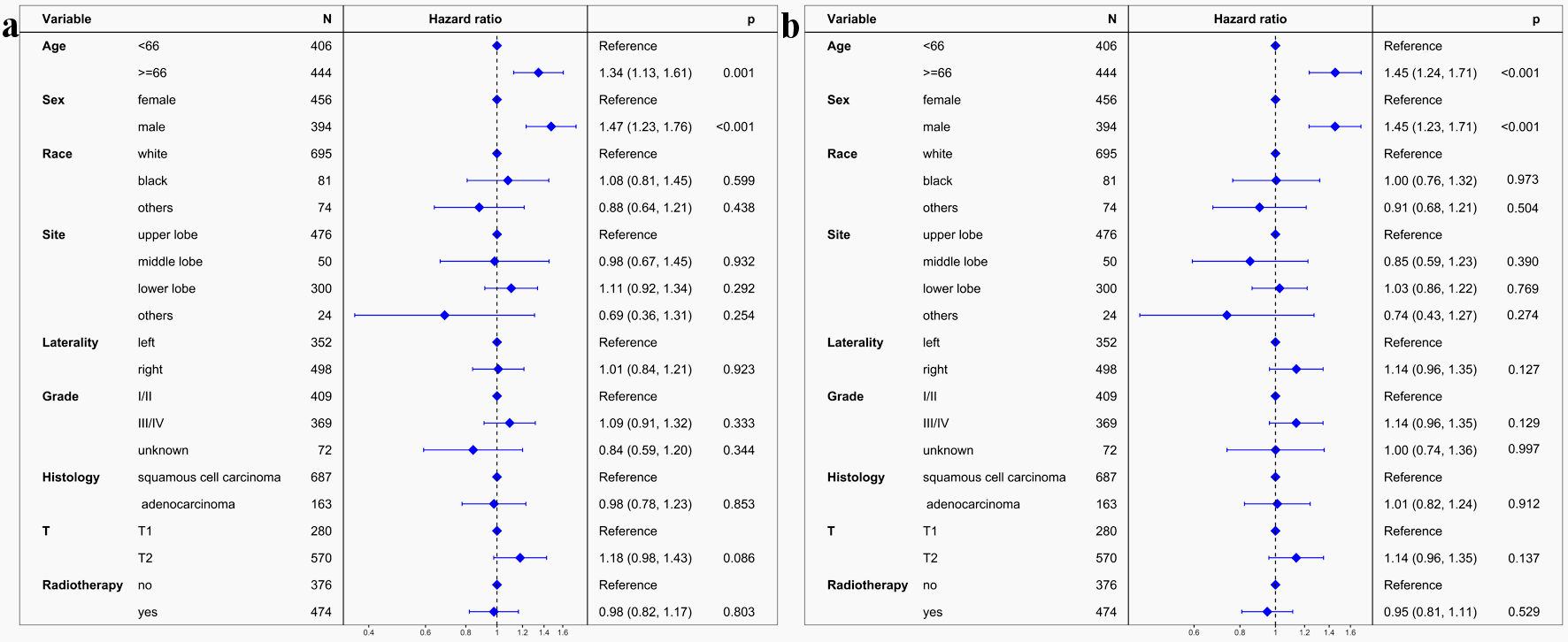 Click for large image | Figure 6. Multivariate regression analysis evaluating various prognostic factors for treatment outcomes in patients with lymph node ratio ≥ 0.29. (a) Cancer-specific survival. (b) Overall survival. LNR: lymph node ratio. |
Similarly, OS did not differ significantly between the non-radiotherapy and radiotherapy subgroups. OS was 38 months in the non-radiotherapy group and 41 months in the radiotherapy group. The 5-year OS rates were 37.6% for the non-radiotherapy group and 40.2% for the radiotherapy group (HR = 0.95; 95% CI: 0.81 - 1.11; P = 0.533) (Fig. 5b). Multivariable Cox regression analysis confirmed no significant independent prognostic impact of radiotherapy on OS (aHR = 0.95, 95% CI: 0.81 - 1.11; P = 0.529) (Fig. 6b).
| Discussion | ▴Top |
This study sought to evaluate the impact of the LNR on treatment outcomes in patients with stage pIIIA-N2 NSCLC after complete resection and adjuvant chemotherapy. A pivotal discovery was the establishment of 0.29 as the optimal LNR cut-off for both CSS and OS using sophisticated restricted cubic spline regression models. This threshold effectively delineates patients into low-risk (LNR < 0.29) and high-risk (LNR ≥ 0.29) categories. Notably, our analysis revealed that postoperative radiotherapy did not significantly enhance CSS or OS in the high-risk group.
Our findings are in consonance with key trials such as CALGB 9734, PORT-C, and Lung ART, which generally discourage routine postoperative radiotherapy for patients with pIIIA-N2 NSCLC following resection and chemotherapy [7-9]. Despite these guidelines, the continued occurrence of high locoregional recurrence rates, ranging from 20% to 60% [38-40] raises questions about the potential role of postoperative radiotherapy in reducing these recurrences [41-47]. While the PORT-C trial observed a slight improvement in 3-year DFS for patients undergoing postoperative radiotherapy [8], and the Lung ART trial reported extended median DFS [7], these findings suggest that specific patient subgroups might benefit from postoperative radiotherapy.
Although postoperative radiotherapy does improve locoregional recurrence-free survival [7-9], this benefit does not appear to extend to DFS and OS. A possible explanation is that the adverse effects on the lung and heart induced by postoperative radiotherapy may offset its survival benefits. Additionally, salvage treatments (such as local radiotherapy or surgery) following locoregional recurrence could enhance survival in patients who did not receive postoperative radiotherapy, leading to comparable OS between postoperative radiotherapy and non-radiotherapy groups.
It is suggested that stage pIIIA-N2 NSCLC patients post complete resection, and adjuvant chemotherapy should receive postoperative radiotherapy based on specific risk prognostic factors [27, 28]. However, the reliance on a single prognostic factor like LNR in determining high-risk patients may be overly simplistic. A more comprehensive approach, integrating multiple factors into an inclusive prognostic model, could provide a more precise identification of patients likely to benefit from postoperative radiotherapy [38, 48].
While our study highlights LNR’s significance as a prognostic indicator, its clinical application must be cautiously approached. The evolving landscape of adjuvant therapies, particularly tyrosine kinase inhibitor therapy for EGFR mutated cases and immunotherapy for EGFR wild-type cases, is crucial [11-14, 49]. Our analysis is constrained by the absence of data on these therapies in the SEER database, underscoring the necessity for further validation in varied clinical contexts.
Future research should initially focus on the patterns of failure post-adjuvant EGFR tyrosine kinase inhibitor therapy and immunotherapy. Subsequent prospective cohort studies comparing treatment outcomes of postoperative radiotherapy and non-radiotherapy in these patients are warranted. Based on these studies, a randomized controlled trial could be conducted to validate the efficacy of postoperative radiotherapy in this specific subgroup.
In conclusion, our study underscores LNR’s prognostic value in stage pIIIA-N2 NSCLC patients following complete resection and adjuvant chemotherapy. An LNR threshold of 0.29 is proposed for effective risk stratification. Although patients with higher LNR exhibit poorer CSS and OS, postoperative radiotherapy did not confer survival benefits in this high-risk cohort. Our study suggests refraining from postoperative radiotherapy in these patients and calls for additional research to identify effective treatments for this subgroup.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Informed consent was waived by the Ethics Committee/IRB of Guangxi Medical University Cancer Hospital.
Author Contributions
Conceptualization: Zu Yi Chen. Methodology: Huan Wei Liang and Yang Liu. Formal analysis: Zu Yi Chen and Huan Wei Liang. Investigation: Yang Liu. Resources: Zu Yi Chen and Huan Wei Liang. Validation: Wei Huang. Writing - original draft preparation: Zu Yi Chen. Writing - review and editing: Xin Bin Pan.
Data Availability
The data are available from the corresponding author upon request.
Abbreviations
NSCLC: non-small cell lung cancer; DFS: disease-free survival; OS: overall survival; EGFR: epidermal growth factor receptor; LNR: lymph node ratio; SEER: the Surveillance, Epidemiology, and End Results; CSS: cancer-specific survival; HR: hazard ratio; CI: confidence interval
| References | ▴Top |
- Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7-33.
doi pubmed - Tan WL, Chua KLM, Lin CC, Lee VHF, Tho LM, Chan AW, Ho GF, et al. Asian thoracic oncology research group expert consensus statement on optimal management of stage III NSCLC. J Thorac Oncol. 2020;15(3):324-343.
doi pubmed - Ettinger DS, Wood DE, Aisner DL, Akerley W, Bauman JR, Bharat A, Bruno DS, et al. NCCN guidelines insights: non-small cell lung cancer, Version 2.2021. J Natl Compr Canc Netw. 2021;19(3):254-266.
doi pubmed - Douillard JY, Rosell R, De Lena M, Carpagnano F, Ramlau R, Gonzales-Larriba JL, Grodzki T, et al. Adjuvant vinorelbine plus cisplatin versus observation in patients with completely resected stage IB-IIIA non-small-cell lung cancer (Adjuvant Navelbine International Trialist Association [ANITA]): a randomised controlled trial. Lancet Oncol. 2006;7(9):719-727.
doi pubmed - Arriagada R, Bergman B, Dunant A, Le Chevalier T, Pignon JP, Vansteenkiste J, International Adjuvant Lung Cancer Trial Collaborative G. Cisplatin-based adjuvant chemotherapy in patients with completely resected non-small-cell lung cancer. N Engl J Med. 2004;350(4):351-360.
doi pubmed - Winton T, Livingston R, Johnson D, Rigas J, Johnston M, Butts C, Cormier Y, et al. Vinorelbine plus cisplatin vs. observation in resected non-small-cell lung cancer. N Engl J Med. 2005;352(25):2589-2597.
doi pubmed - Le Pechoux C, Pourel N, Barlesi F, Lerouge D, Antoni D, Lamezec B, Nestle U, et al. Postoperative radiotherapy versus no postoperative radiotherapy in patients with completely resected non-small-cell lung cancer and proven mediastinal N2 involvement (Lung ART): an open-label, randomised, phase 3 trial. Lancet Oncol. 2022;23(1):104-114.
doi pubmed - Hui Z, Men Y, Hu C, Kang J, Sun X, Bi N, Zhou Z, et al. Effect of postoperative radiotherapy for patients with pIIIA-N2 non-small cell lung cancer after complete resection and adjuvant chemotherapy: the phase 3 PORT-C randomized clinical trial. JAMA Oncol. 2021;7(8):1178-1185.
doi pubmed pmc - Perry MC, Kohman LJ, Bonner JA, Gu L, Wang X, Vokes EE, Green MR. A phase III study of surgical resection and paclitaxel/carboplatin chemotherapy with or without adjuvant radiation therapy for resected stage III non-small-cell lung cancer: Cancer and Leukemia Group B 9734. Clin Lung Cancer. 2007;8(4):268-272.
doi pubmed - Wang SF, Mao NQ, Zhao WH, Pan XB. Postoperative radiotherapy in pIIIA-N2 non-small cell lung cancer after complete resection and adjuvant chemotherapy: A meta-analysis. Medicine (Baltimore). 2022;101(28):e29550.
doi pubmed - Herbst RS, Wu YL, John T, Grohe C, Majem M, Wang J, Kato T, et al. Adjuvant osimertinib for resected EGFR-mutated stage IB-IIIA non-small-cell lung cancer: updated results from the phase III randomized ADAURA trial. J Clin Oncol. 2023;41(10):1830-1840.
doi pubmed pmc - Zhong WZ, Wang Q, Mao WM, Xu ST, Wu L, Wei YC, Liu YY, et al. Gefitinib versus vinorelbine plus cisplatin as adjuvant treatment for stage II-IIIA (N1-N2) EGFR-mutant NSCLC: final overall survival analysis of CTONG1104 phase III trial. J Clin Oncol. 2021;39(7):713-722.
doi pubmed pmc - Felip E, Altorki N, Zhou C, Vallieres E, Martinez-Marti A, Rittmeyer A, Chella A, et al. Overall survival with adjuvant atezolizumab after chemotherapy in resected stage II-IIIA non-small-cell lung cancer (IMpower010): a randomised, multicentre, open-label, phase III trial. Ann Oncol. 2023;34(10):907-919.
doi pubmed - O'Brien M, Paz-Ares L, Marreaud S, Dafni U, Oselin K, Havel L, Esteban E, et al. Pembrolizumab versus placebo as adjuvant therapy for completely resected stage IB-IIIA non-small-cell lung cancer (PEARLS/KEYNOTE-091): an interim analysis of a randomised, triple-blind, phase 3 trial. Lancet Oncol. 2022;23(10):1274-1286.
doi pubmed - Rizzo A, Cusmai A, Giovannelli F, Acquafredda S, Rinaldi L, Misino A, Montagna ES, et al. Impact of proton pump inhibitors and histamine-2-receptor antagonists on non-small cell lung cancer immunotherapy: a systematic review and meta-analysis. Cancers (Basel). 2022;14(6):1404.
doi pubmed pmc - Mollica V, Rizzo A, Marchetti A, Tateo V, Tassinari E, Rosellini M, Massafra R, et al. The impact of ECOG performance status on efficacy of immunotherapy and immune-based combinations in cancer patients: the MOUSEION-06 study. Clin Exp Med. 2023;23(8):5039-5049.
doi pubmed - Santoni M, Rizzo A, Mollica V, Matrana MR, Rosellini M, Faloppi L, Marchetti A, et al. The impact of gender on The efficacy of immune checkpoint inhibitors in cancer patients: The MOUSEION-01 study. Crit Rev Oncol Hematol. 2022;170:103596.
doi pubmed - Rizzo A. Identifying optimal first-line treatment for advanced non-small cell lung carcinoma with high PD-L1 expression: a matter of debate. Br J Cancer. 2022;127(8):1381-1382.
doi pubmed pmc - Santoni M, Rizzo A, Kucharz J, Mollica V, Rosellini M, Marchetti A, Tassinari E, et al. Complete remissions following immunotherapy or immuno-oncology combinations in cancer patients: the MOUSEION-03 meta-analysis. Cancer Immunol Immunother. 2023;72(6):1365-1379.
doi pubmed - Huber RM, De Ruysscher D, Hoffmann H, Reu S, Tufman A. Interdisciplinary multimodality management of stage III nonsmall cell lung cancer. Eur Respir Rev. 2019;28(152):190024.
doi pubmed pmc - Postmus PE, Kerr KM, Oudkerk M, Senan S, Waller DA, Vansteenkiste J, Escriu C, et al. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28(suppl_4):iv1-iv21.
doi pubmed - Miller ED, Fisher JL, Haglund KE, Grecula JC, Xu-Welliver M, Bertino EM, He K, et al. The addition of chemotherapy to radiation therapy improves survival in elderly patients with stage III non-small cell lung cancer. J Thorac Oncol. 2018;13(3):426-435.
doi pubmed pmc - Davidoff AJ, Gardner JF, Seal B, Edelman MJ. Population-based estimates of survival benefit associated with combined modality therapy in elderly patients with locally advanced non-small cell lung cancer. J Thorac Oncol. 2011;6(5):934-941.
doi pubmed - Curran WJ, Jr., Paulus R, Langer CJ, Komaki R, Lee JS, Hauser S, Movsas B, et al. Sequential vs. concurrent chemoradiation for stage III non-small cell lung cancer: randomized phase III trial RTOG 9410. J Natl Cancer Inst. 2011;103(19):1452-1460.
doi pubmed pmc - Bradley JD, Paulus R, Komaki R, Masters G, Blumenschein G, Schild S, Bogart J, et al. Standard-dose versus high-dose conformal radiotherapy with concurrent and consolidation carboplatin plus paclitaxel with or without cetuximab for patients with stage IIIA or IIIB non-small-cell lung cancer (RTOG 0617): a randomised, two-by-two factorial phase 3 study. Lancet Oncol. 2015;16(2):187-199.
doi pubmed pmc - Yoon SM, Shaikh T, Hallman M. Therapeutic management options for stage III non-small cell lung cancer. World J Clin Oncol. 2017;8(1):1-20.
doi pubmed pmc - Zhou S, Zhai Y, Zhao K, Men Y, Meng X, Hui Z. Real world practice of postoperative radiotherapy for patients with completely resected pIIIA-N2 non-small cell lung cancer: a national survey of radiation oncologists in China. Radiat Oncol. 2023;18(1):17.
doi pubmed pmc - Zhu M, Li S, Yuan L, Liu S, Li J, Zhang D, Chen J, et al. The high-risk features and effect of postoperative radiotherapy on survival for patients with surgically treated stage IIIA-N2 non-small cell lung cancer. World J Surg Oncol. 2023;21(1):238.
doi pubmed pmc - Mei W, Yao W, Song Z, Jiao W, Zhu L, Huang Q, An C, et al. Development and validation of prognostic nomogram for T(1-3)N(0)M(0) non-small cell lung cancer after curative resection. BMC Cancer. 2023;23(1):715.
doi pubmed pmc - Zhu Z, Song Z, Jiao W, Mei W, Xu C, Huang Q, An C, et al. A large real-world cohort study of examined lymph node standards for adequate nodal staging in early non-small cell lung cancer. Transl Lung Cancer Res. 2021;10(2):815-825.
doi pubmed pmc - Thomas PA. Intraoperative lymph-node assessment during NSCLC surgery: the need for standardisation and quality evaluation. Lancet Oncol. 2019;20(1):23-25.
doi pubmed - Feng S, Liu X, Huang B, Shi J, Zhang H. The effect of examined lymph nodes and lymph node ratio on pathological nodal classification in the lung adenosquamous carcinoma after lobectomy. Front Surg. 2022;9:909810.
doi pubmed pmc - Wang SF, Mao NQ, Huang JQ, Pan XB. Lymph node ratio enhances predictive value for treatment outcomes in patients with non-small cell lung cancer undergoing surgery: a retrospective cohort study. J Cancer. 2024;15(2):466-472.
doi pubmed pmc - Zhu F, Wang H, Ashamalla H. The significance of lymph node ratio and total lymph nodes examined in determining the indications of adjuvant radiation in pN2 non-small cell lung cancer. Clin Lung Cancer. 2022;23(6):e384-e393.
doi pubmed - Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8(5):551-561.
doi pubmed - Govindarajulu US, Spiegelman D, Thurston SW, Ganguli B, Eisen EA. Comparing smoothing techniques in Cox models for exposure-response relationships. Stat Med. 2007;26(20):3735-3752.
doi pubmed - Lee DH, Keum N, Hu FB, Orav EJ, Rimm EB, Willett WC, Giovannucci EL. Predicted lean body mass, fat mass, and all cause and cause specific mortality in men: prospective US cohort study. BMJ. 2018;362:k2575.
doi pubmed pmc - Xu L, Xie HN, Chen XK, Bi N, Qin JJ, Li Y. Patient prognostic scores and association with survival improvement offered by postoperative radiotherapy for resected IIIA/N2 non-small cell lung cancer: A population-based study. Thorac Cancer. 2021;12(6):760-767.
doi pubmed pmc - Zhu L, Xia B, Ma S. Postoperative radiotherapy for patients with completely resected stage IIIA-N2 non-small cell lung cancer: opt-in or opt-out. Thorac Cancer. 2022;13(5):659-663.
doi pubmed pmc - Mahvi DA, Liu R, Grinstaff MW, Colson YL, Raut CP. Local cancer recurrence: the realities, challenges, and opportunities for new therapies. CA Cancer J Clin. 2018;68(6):488-505.
doi pubmed pmc - Dai H, Hui Z, Ji W, Liang J, Lu J, Ou G, Zhou Z, et al. Postoperative radiotherapy for resected pathological stage IIIA-N2 non-small cell lung cancer: a retrospective study of 221 cases from a single institution. Oncologist. 2011;16(5):641-650.
doi pubmed pmc - Corso CD, Rutter CE, Wilson LD, Kim AW, Decker RH, Husain ZA. Re-evaluation of the role of postoperative radiotherapy and the impact of radiation dose for non-small-cell lung cancer using the National Cancer Database. J Thorac Oncol. 2015;10(1):148-155.
doi pubmed - Robinson CG, Patel AP, Bradley JD, DeWees T, Waqar SN, Morgensztern D, Baggstrom MQ, et al. Postoperative radiotherapy for pathologic N2 non-small-cell lung cancer treated with adjuvant chemotherapy: a review of the National Cancer Data Base. J Clin Oncol. 2015;33(8):870-876.
doi pubmed pmc - Sakib N, Li N, Zhu X, Li D, Li Y, Wang H. Effect of postoperative radiotherapy on outcome in resectable stage IIIA-N2 non-small-cell lung cancer: an updated meta-analysis. Nucl Med Commun. 2018;39(1):51-59.
doi pubmed - Billiet C, Decaluwe H, Peeters S, Vansteenkiste J, Dooms C, Haustermans K, De Leyn P, et al. Modern post-operative radiotherapy for stage III non-small cell lung cancer may improve local control and survival: a meta-analysis. Radiother Oncol. 2014;110(1):3-8.
doi pubmed - Lei T, Li J, Zhong H, Zhang H, Jin Y, Wu J, Li L, et al. Postoperative radiotherapy for patients with resectable stage III-N2 non-small cell lung cancer: a systematic review and meta-analysis. Front Oncol. 2021;11:680615.
doi pubmed pmc - Liu J, Ladbury C, Kim J, Raz D, Erhunmwunsee L, West HJ, Williams T, et al. Postoperative radiation therapy should be used for completely resected stage III-N2 NSCLC in select patients. J Thorac Oncol. 2022;17(2):194-196.
doi pubmed - Zhang CC, Hou RP, Xia WY, Zeng WQ, Liu J, Wang JM, Lv CX, et al. Prognostic index for estimating the survival benefit of postoperative radiotherapy in pathologic N2 non-small cell lung cancer: A real-world validation study. Lung Cancer. 2021;156:100-108.
doi pubmed - Wu YL, Tsuboi M, He J, John T, Grohe C, Majem M, Goldman JW, et al. Osimertinib in resected EGFR-mutated non-small-cell lung cancer. N Engl J Med. 2020;383(18):1711-1723.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Oncology is published by Elmer Press Inc.


