| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website http://www.wjon.org |
Case Report
Volume 7, Number 5-6, December 2016, pages 119-123
Radiation-Induced Malignancies: Our Experiences With Five Cases
Gunjesh Kumar Singha, c, Vikas Yadava, Pragya Singhb, K. T. Bhowmika
aDepartment of Radiotherapy, VMMC and Safdarjung Hospital, New Delhi 110029, India
bDepartment of Pathology, VMMC and Safdarjung Hospital, New Delhi 110029, India
cCorresponding Author: Gunjesh Kumar Singh, Department of Radiotherapy, VMMC and Safdarjung Hospital, New Delhi 110029, India
Manuscript accepted for publication December 20, 2016
Short title: Radiation-Induced Malignancies
doi: https://doi.org/10.14740/wjon991w
| Abstract | ▴Top |
Radiotherapy is one of the modalities of treatment of malignancies. Radiation-induced malignancies (RIMs) are late complications of radiotherapy, seen among the survivors of both adult and pediatric cancers. Mutagenesis of normal tissues is the likely basis for RIMs. Till date, RIM cannot be differentiated from primary cancers. We present a series of five patients who were treated at our institute between 2002 and 2016 and were subsequently diagnosed with RIM. Out of five patients, there were two cases of sarcomas, two of carcinomas and one neuroendocrine carcinoma of tongue (rare entity). Separate treatment guidelines are not available for RIM, so the treatment given was same as primary malignancies.
Keywords: Radiation-induced malignancies; Sarcomas; Neuroendocrine carcinoma
| Introduction | ▴Top |
Radiation is increasingly being used as a diagnostic tool for various diseases and as a treatment modality of various cancerous and non-cancerous conditions. Radiation-induced malignancies (RIMs) are one of the rare but serious potential side effects of radiation. Radiation-induced mutation of normal tissues is one of the proposed mechanisms but exact pathogenesis is still unknown. It can be rightly considered a “two-edged sword” as treatment by radiation is itself causing cancer.
We report five cases of RIM treated and analyzed for outcome at our institute.
| Case Reports | ▴Top |
Case 1
A 65-year-old male presented in January 2002 with lump in right breast for 2 months. He was diagnosed with carcinoma breast, was operated and received six cycles of adjuvant chemotherapy with cyclophosphamide, adriamycin, 5-flurouracil (CAF) and external beam radiotherapy (50 Gy in 25 fractions) to chest wall, axilla, supraclavicular and internal mammary portals by cobalt 60. Patient was asymptomatic during follow-up. In June 2016, patient presented with complaints of difficulty in swallowing solid and semisolid food. Upper gastrointestinal endoscopy showed an ulcerative growth with luminal narrowing at a distance of about 22 cm from incisor. Biopsy was done and histopathological examination (HPE) revealed moderately differentiated squamous cell carcinoma (MDSCC) (Fig. 1a). Whole body positron emission tomography-contrast-enhanced computed tomography (PET-CECT) revealed fluorodeoxyglucose (FDG) avid mass lesion in esophagus, about 3.5 cm in craniocaudal dimension (Fig. 1b). According to the age and Karnofsky performance score (KPS) 50, patient was planned for palliative radiotherapy to esophagus, but the patient expired before receiving treatment.
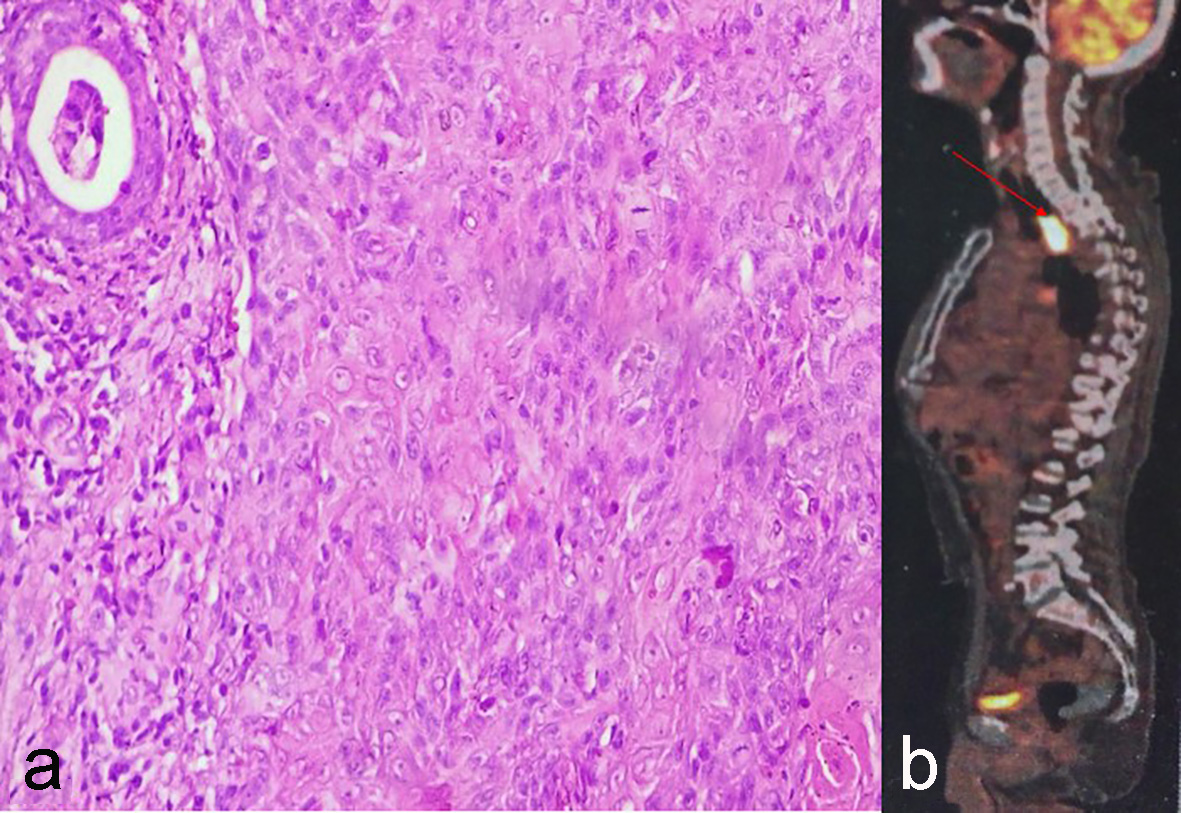 Click for large image | Figure 1. (a) Moderately differentiated squamous cell carcinoma. (b) PET-CECT showing FDG avid mass lesion in esophagus at level of D2-D4. |
Case 2
A 45-year-old premenopausal female presented in the outpatient department with complaints of on and off bleeding per vaginum (PV) and foul smelling discharge since 1 month (August 2003). On local examination, there was a cervical growth with right-sided parametrial involvement. Biopsy from cervical growth showed MDSCC and a final diagnosis of carcinoma cervix, FIGO stage IIB was made. Patient was treated with concurrent chemotherapy with cisplatin and radiotherapy to whole pelvis to a dose of 50 Gy in 25 fractions by four-field box technique followed by high-dose-rate (HDR) intracavitary radiotherapy (ICRT) 7 Gy in 3 fractions after taking proper consent. On response assessment, patient was in complete remission and remained so during follow-up for 12 years.
After 12 years, in August 2015, patient complained of dull aching pain abdomen in suprapubic region. Magnetic resonance imaging (MRI) of abdomen revealed a large heterogenous mass lesion with solid cystic areas completely replacing the uterine parenchyma (Fig. 2a).
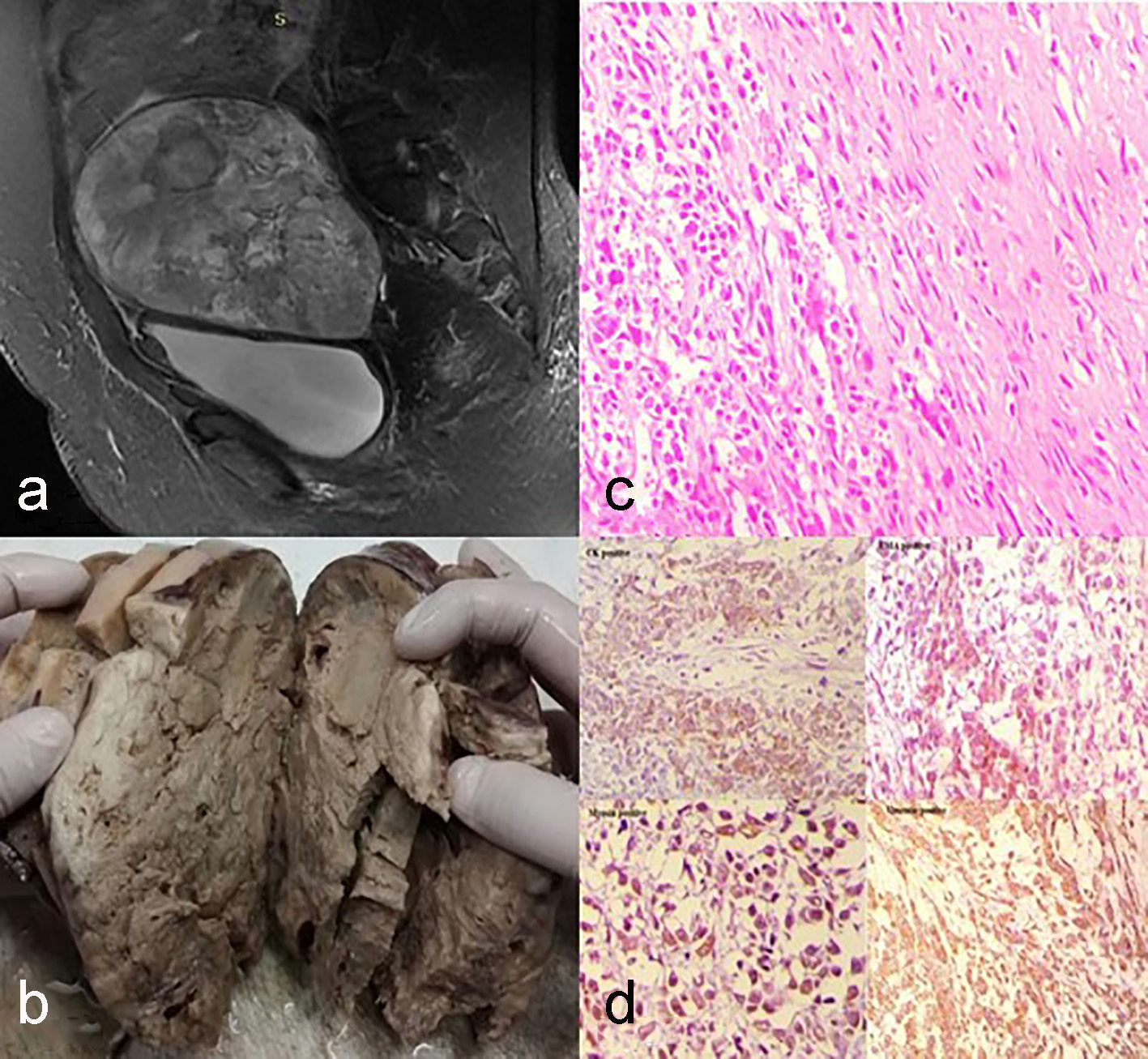 Click for large image | Figure 2. (a) MRI of abdomen shows uterine parenchyma is completely replaced by a large heterogenous mass lesion having solid and cystic areas, measuring 11 × 13.1 × 14.7 cm. (b) On gross examination of uterus specimen, a large tumor measuring 17 × 14 × 7 cm was identified. (c) Histopathological examination is showing a cellular tumour consisting of oval to elongated and polygonal cells. The elongated cells are arranged in palisading and haphazard pattern. The polygonal cells at places are forming ill-defined trabecular and glandular patterns (× 40). (d) Immunohistochemistry (IHC) showing positivity for vimentin, myosin, CK and focally for EMA (× 40). |
Case was discussed in multidisciplinary clinic and total abdominal hysterectomy + bilateral salpingo oophorectomy (TAH + BSO) with bilateral pelvic lymphadenectomy was performed after proper metastatic workup. Histopathology examination of hysterectomy specimen showed presence of a large tumor (17 × 14 × 7 cm) in uterus on gross examination (Fig. 2b) with microscopic features of carcinosarcoma uterus (Fig. 2c, d) reaching up to the serosa and involving the inferior resected margin. As already full-dose radiotherapy was given for carcinoma cervix, re-irradiation was not possible. Considering poor prognosis of the tumor and propensity for distant metastasis, patient was advised adjuvant chemotherapy.
Patient is currently on adjuvant chemotherapy with ifosfamide and paclitaxel, and has received three cycles and is tolerating well.
Case 3
A 46-year-old male presented in December 2009 with chief complains of pain and difficulty in swallowing since 2 months. Patient was a chronic smoker. On examination, there was an ulceroproliferative growth (UPG) involving the base of tongue. HPE revealed MDSCC. CECT showed heterogeneously enhancing mass involving base of tongue with bilateral cervical lymphadenopathy and tumor was accordingly staged T3N2CM0. Patient completed concurrent chemoradiation (66 Gy in 33 fractions with cisplatin 40 mg/m2 weekly) in January 2010 and remained in complete remission for about 6 years. In June 2016, he presented with complaint of dysphagia. Local examination showed a proliferative growth in the posterior 1/3 of tongue. CECT from base of skull to thoracic inlet showed a 3 × 2 × 1 cm mass in right side base of tongue with involvement of the floor of mouth (Fig. 3a). Biopsy from the lesion revealed neuroendocrine carcinoma (Fig. 3b, c). Metastatic workup showed liver metastasis. Patient has been planned for combination chemotherapy with 5-florouracil, dacarbazine and epirubicin.
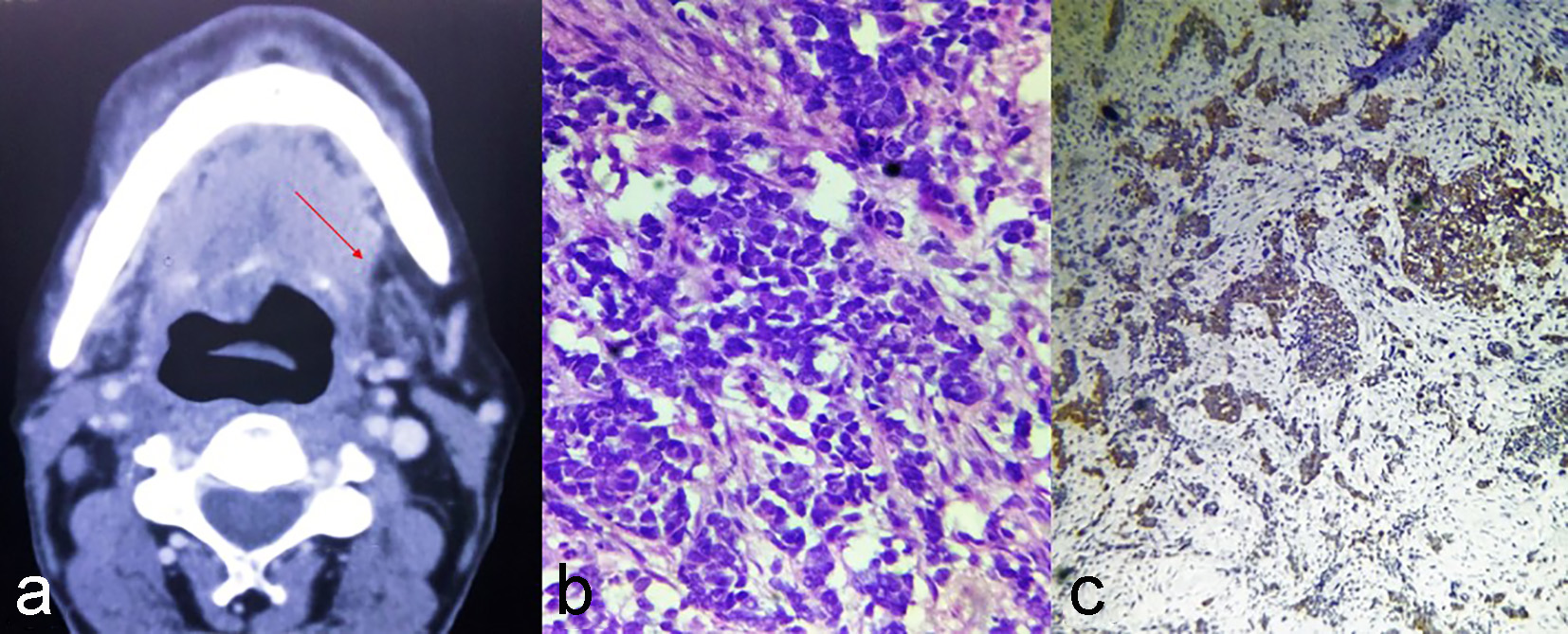 Click for large image | Figure 3. (a) CECT neck showing mass of size 3 × 2 × 1 cm on right side base of tongue with floor of mouth involvement. (b) The tumour cells are arranged in small nests. The cells have round to oval hyperchromatic nuclei with scant cytoplasm. (c) IHC showing positivity for neuron specific enolase. |
Case 4
A 55-year-old male presented in June 2011, with history of ulcer in right buccal mucosa since 2 months. Patient was operated and HPE revealed well-differentiated squamous cell carcinoma, buccal mucosa. Concurrent chemoradiation was given (66 Gy in 33 fractions with cisplatin 40 mg/m2 weekly) in August 2011 for postoperative microscopic residual disease. The disease free duration was 4 years. In February 2015, he developed ulcer over right buccal mucosa for which wide local excision was done in May 2015. HPE showed leiomyosarcoma of right side buccal mucosa. Patient did not give consent for re-irradiation and was not fit for adriamycin-based chemotherapy because of low ejection fraction of < 40%. Patient was wishful for homeopathic medicines and remained on follow-up. His last review in the department was in June 2015.
Case 5
A 72-year-old male presented in March 2013 with chief complains of difficulty in breathing, swallowing and foreign body sensation in throat since 2 months. On indirect laryngoscopy, there was UPG in the right side vallecula, epiglottis and right side pyriform sinus. Biopsy from the growth was taken which showed poorly differentiated squamous cell carcinoma (PDSCC). CECT neck showed an enhancing mass measuring 2.8 × 2.5 × 1.6 cm in right side supraglottic larynx (Fig. 4a). Patient received concurrent chemoradiation (66 Gy in 33 fractions with cisplatin 40 mg/m2 weekly) which was completed in May 2013 and remained in complete remission for about 3 years. In June 2016, he presented with complains of swelling over left cheek since 2 months. On examination, there was a 4 × 3 cm UPG involving left lower gingivobuccal sulcus (GBS) and adjacent buccal mucosa. HPE report showed PDSCC (Fig. 4b). CECT report showed 3.1 × 2.6 × 2 cm enhancing mass in left lower GBS and extending up to skin with no evidence of previous malignancy (Fig. 4c). Patient denied salvage surgery and is being treated with re-irradiation (concurrent chemoradiation).
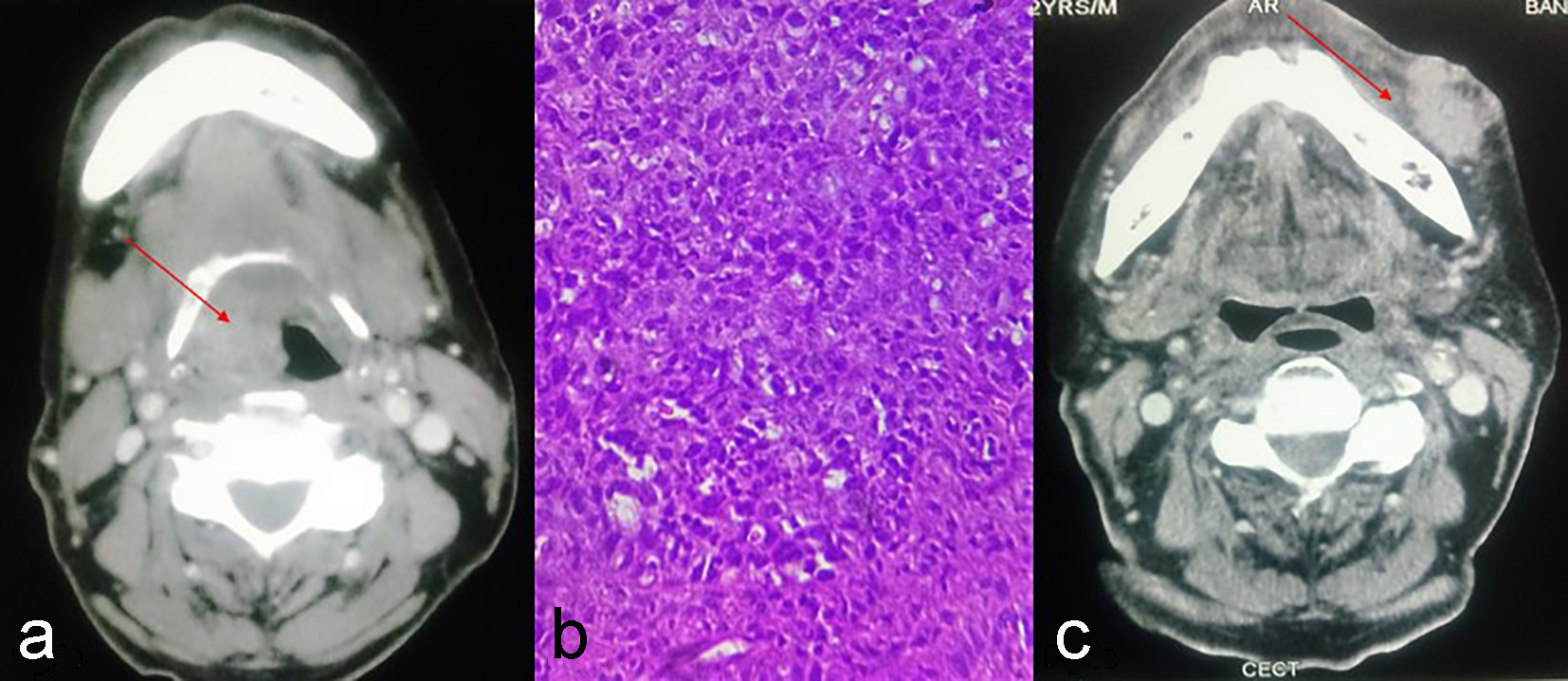 Click for large image | Figure 4. (a) CECT of neck showing enhancing mass measuring in right side supraglottic larynx. (b) Poorly differentiated squamous cell carcinoma. (c) CECT showing enhancing mass in left lower GBS and extending up to skin. |
| Discussion | ▴Top |
RIM was first defined by Cahan et al [1] in 1948. The modified Cahan’s criteria for diagnosis are: 1) An RIM must have arisen in an irradiated field. 2) A sufficient latent period, preferably longer than 4 years, must have elapsed between the initial irradiation and the alleged induced malignancy. 3) The treated tumor must have been biopsied. The alleged induced tumor must have been biopsied. The two tumors must be of different histology. 4) The tissue in which the alleged induced tumor arose must have been normal (i.e., metabolically and genetically normal) prior to radiation exposure.
These criteria have a good reference value when a cancer is suspected to be secondary RIM.
Concept of RIM comes from survivors of the atom bomb attacks on Japan. The overall risk of fatal cancers in atom bomb survivors to be 8%/Gy was concluded by Hall and Wuu [2]. Till date, histology of RIM cannot be distinguished from natural occurring tumor. Molecular forensics may have a role regarding its diagnosis in future [3].
Factors affecting RIM are as follows: 1) Dose and linear energy transfer (LET) - carcinoma and leukemias are common at low dose while sarcomas are predominantly seen arising in tissues or organ receiving high-dose radiation [2]. 2) Energy - RIM commonly seen with orthovoltage in comparison to megavoltage radiotherapy [4]. 3) Age - children are more prone to RIM in comparison to adults [5]. 4) Hereditary disposition like neurofibromatosis I (NF1), familial retinoblastoma, tuberous sclerosis and various chemotherapeutic agents can increase the risk of cancer development after radiation exposure [6, 7]. 5) Treatment modalities - RIMs are common in intensity-modulated radiation therapy (IMRT) in comparison to conventional mode of radiotherapy [2, 8]. Decrease in field size decreases the incidence of second malignancy [9].
Radiation-induced genomic injury is one of the proposed mechanisms for radiation-induced tumorigenesis in normal tissues. The bystander effect is a phenomenon, in which untreated cells demonstrate abnormalities mimicking exposure, such as chromosomal instability after irradiation [10]. We presented five cases of RIM (summarized in Table 1). Minimum latent period in our case series was about 3 years while maximum was 14 years. All malignancies were in field of radiotherapy except one, which was PDSCC of right side lower GBS, which developed after treatment of supraglottic carcinoma. There were two cases of sarcomas, two of carcinomas and one neuroendocrine carcinoma of tongue (rare entity); three out of five cases are currently receiving treatment.
 Click to view | Table 1. Our Five Cases of Radiation-Induced Malignancies |
Conclusion
Radiotherapy is an important treatment modality in oncological care. RIMs are considered as one of the most significant and life-threatening late complications of radiotherapy. Radiation has widespread use in diagnostic, therapeutic and commercial fields, thereby increasing the incidence. There are no current well-defined criteria to differentiate primary malignancy and RIM. Molecular forensics may be looked upon as a potential field for future studies on RIM including their pathogenesis and behavior.
Conflicts of Interest
Authors have no conflicts of interest.
| References | ▴Top |
- Cahan WG, Woodard HQ, Higinbotham NL, Stewart FW, Coley BL. Sarcoma arising in irradiated bone: report of eleven cases. 1948. Cancer. 1998;82(1):8-34.
doi - Hall EJ, Wuu CS. Radiation-induced second cancers: the impact of 3D-CRT and IMRT. Int J Radiat Oncol Biol Phys. 2003;56(1):83-88.
doi - Bogni A, Cheng C, Liu W, Yang W, Pfeffer J, Mukatira S, French D, et al. Genome-wide approach to identify risk factors for therapy-related myeloid leukemia. Leukemia. 2006;20(2):239-246.
doi pubmed - Potish RA, Dehner LP, Haselow RE, Kim TH, Levitt SH, Nesbit M. The incidence of second neoplasms following megavoltage radiation for pediatric tumors. Cancer. 1985;56(7):1534-1537.
doi - Neglia JP, Robison LL, Stovall M, Liu Y, Packer RJ, Hammond S, Yasui Y, et al. New primary neoplasms of the central nervous system in survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Natl Cancer Inst. 2006;98(21):1528-1537.
doi pubmed - Sage J. The retinoblastoma tumor suppressor and stem cell biology. Genes Dev. 2012;26(13):1409-1420.
doi pubmed - Kleinerman RA. Radiation-sensitive genetically susceptible pediatric sub-populations. Pediatr Radiol. 2009;39(Suppl 1):S27-31.
doi pubmed - Hall EJ. Intensity-modulated radiation therapy, protons, and the risk of second cancers. Int J Radiat Oncol Biol Phys. 2006;65(1):1-7.
doi pubmed - Sasse S, Klimm B, Gorgen H, Fuchs M, Heyden-Honerkamp A, Lohri A, Koch O, et al. Comparing long-term toxicity and efficacy of combined modality treatment including extended- or involved-field radiotherapy in early-stage Hodgkin's lymphoma. Ann Oncol. 2012;23(11):2953-2959.
doi pubmed - Mothersill C, Seymour CB. Radiation-induced bystander effects - implications for cancer. Nat Rev Cancer. 2004;4(2):158-164.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Oncology is published by Elmer Press Inc.


