| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://www.wjon.org |
Original Article
Volume 15, Number 4, August 2024, pages 625-639
Comparison of Outcomes Between Partial and Radical Laparoscopic Nephrectomy for Localized Renal Tumors Larger Than Four Centimeters: A Systematic Review and Meta-Analysis
Bao Nan Donga, Jie Songa, Wen Li Yanga, Hui Zhana, b, Ting Luana, Jian Song Wanga
aUrology Surgery Department, The Second Affiliated Hospital of Kunming Medical University, Kunming, Yunnan, China
bCorresponding Author: Hui Zhan, Urology Surgery Department, The Second Affiliated Hospital of Kunming Medical University, Wuhua District, Kunming 650101, Yunnan, China
Manuscript submitted March 12, 2024, accepted May 25, 2024, published online July 5, 2024
Short title: Partial and Radical Nephrectomy for Renal Tumors
doi: https://doi.org/10.14740/wjon1866
| Abstract | ▴Top |
Background: Earlier studies have juxtaposed different laparoscopic methods for treating renal tumors; however, extensive evidence with a particular focus on large kidney tumors remains lacking. The objective of this meta-analysis was to assess the perioperative outcomes, kidney performance, and cancer-related results of laparoscopic partial nephrectomy (LPN) versus laparoscopic radical nephrectomy (LRN) for treating extensive, localized, non-metastatic kidney tumors (cT1b-cT2N0M0).
Methods: We systematically searched multiple databases from database inception until December 2023 for relevant studies. Selected data were analyzed with the Cochrane Collaboration’s Review Manager 5.4 software using a random-effects model. Outcomes were expressed as odds ratios and weighted mean differences with 95% confidence intervals, considering a P value of < 0.05 as significant.
Results: Data from nine studies encompassing 1,303 patients (529 LPN, 774 LRN) revealed that LPN was associated with lengthier surgeries and increased blood loss compared to LRN. While LPN exhibited higher postoperative complication rates, the disparity did not reach statistical significance. LPN led to improved postoperative renal function, manifesting as a reduced estimated glomerular filtration rate (eGFR) decline and fewer incidents of new chronic kidney disease cases. Both groups demonstrated comparable tumor recurrence and overall mortality rates, but LPN exhibited significantly lower cancer-specific mortality rates.
Conclusions: LPN, despite longer operative times and greater intraoperative blood loss, was found to be superior to LRN in preserving postoperative renal function. Oncologically, LPN and LRN have comparable overall mortality rates, but LPN showed a significant advantage in terms of lower cancer-specific mortality rates.
Keywords: Laparoscopy; Nephrectomy; Kidney neoplasms; Systematic review; Meta-analysis
| Introduction | ▴Top |
According to the current TNM staging system, localized renal tumors are classified as small-volume renal tumors (≤ 4 cm) in stage cT1a and large-volume renal tumors (> 4 cm) in stages cT1b and cT2 based on the tumor size. Despite ongoing debates, this classification proves instrumental in guiding clinical decisions [1]. With advancements in imaging and increased awareness, there is a notable rise in cT1a diagnoses, while tumors exceeding 4 cm remain consistently prevalent [2]. Smaller renal tumors increasingly receive less invasive treatments, such as radiofrequency ablation, whereas larger tumors, still a predominant diagnosis, are primarily addressed through surgical interventions. The evolution of laparoscopic techniques has expanded the utilization of both laparoscopic partial nephrectomy (LPN) and laparoscopic radical nephrectomy (LRN) for larger tumors [3], with a specific focus on preserving renal units and enhancing patient survival. Previous research predominantly concentrated on small tumors [4, 5], leaving a void in comprehensive reviews addressing the efficacy of laparoscopic treatments for renal tumors exceeding 4 cm. This study aimed to bridge this gap by conducting a systematic review and meta-analysis to compare the outcomes of LPN and LRN for large renal tumors (> 4 cm, cT1b-cT2N0M0).
| Materials and Methods | ▴Top |
This article was written following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 Statement [6] and has been registered in PROSPERO (registration ID: CRD42023494417). The Institutional Review Board approval, and ethical compliance are not applicable to this study because it involves the synthesis and citation of existing research and does not include new experimental work with human participants or patient data.
Search strategy
We searched databases including PubMed, Cochrane Library, and EMBASE, with the search timeline spanning from the database inception until December 2023, and we limited the language of the retrieved literature to English. During the search process, we constructed a search strategy using patient (P), intervention (I), and control (C). In PubMed and Cochrane Library, we used MeSH terms “kidney neoplasms”, “nephrectomy”, and “laparoscopy” along with their synonyms and related terms, incorporating synonyms for both “partial” and “radical”. In EMBASE, we referred to the explode term in EMTREE “kidney cancer”, “partial nephrectomy (PN)”, “radical nephrectomy (RN)”, and “laparoscopy” and synonyms of each term (Supplementary Material 1, www.wjon.org). To avoid missing relevant studies, we also screened the references of studies containing PN and RN comparison cohorts.
Study selection
The inclusion criteria for the literature were established according to the PICOS principles. 1) Patients (P): patients were individuals who were preoperatively diagnosed with unilateral, solitary, large-volume (maximum diameter > 4 cm) renal occupying lesions (cT1b-cT2N0M0) without local or distant metastasis identified on imaging but were postoperatively confirmed as having renal malignancies (regardless of the specific pathological type) through pathological examination; 2) Intervention (I): The intervention was LPN (e.g., conventional laparoscopy, three-dimensional (3D)/ultra-clear laparoscopy, hand-assisted laparoscopy, and robot-assisted laparoscopy); 3) Control (C): The control intervention was LRN (e.g., conventional laparoscopy, 3D/ultra-clear laparoscopy, hand-assisted laparoscopy, and robot-assisted laparoscopy); 4) Outcomes (O): This included at least one of the following outcomes: perioperative outcomes (e.g., surgical time, intraoperative blood loss, and perioperative complications), renal function outcomes (e.g., postoperative renal function decline and increase in the number of patients with chronic kidney disease (CKD)), and oncological outcomes (e.g., recurrence and metastasis rates, overall mortality (OM), and cancer-specific mortality (CSM)); 5) Study type (S): retrospective case-control study.
The exclusion criteria for the literature were as follows: non-comparative studies, case reports or case series, non-research articles (such as reviews, editorial comments, conference papers, and conference abstracts), meta-analyses, studies lacking necessary data for this research, and ongoing studies with unreported results.
Data collection
Two authors conducted an independent review of the literature, adhering to predefined inclusion and exclusion criteria, and sought the opinion of a third author to address any disagreements. Relevance was initially assessed based on titles and abstracts, with full-text reviews employed for cases that lacked clarity. A fourth author then conducted an independent review of the ultimately selected literature.
Two authors independently extracted data from the included studies, initially focusing on general details such as the first author, publication year, country or region, and study duration. Subsequently, they documented demographic information, encompassing age, body mass index (BMI), sex, cohort size, tumor location, size, clinical stage, preoperative renal function, and follow-up duration. Perioperative details, including operative time, blood loss, postoperative complications (classified using the Clavien-Dindo system), pathological outcomes, and the presence of positive margins, were also collected. Additionally, renal function outcomes, such as postoperative estimated glomerular filtration rate (eGFR) decline and the incidence of CKD, were recorded. Oncological results, encompassing recurrence rates, OM, and CSM, were included in the data extraction process. The validation of the extracted data was carried out independently by other authors.
Risk of bias assessment
The first author conducted a quality assessment of the included literature using the ROBINS-I tool [7], which includes seven dimensions, namely 1) Bias due to confounding; 2) Bias in selection of participants into the study; 3) Bias in classification of interventions; 4) Bias due to deviations from intended interventions; 5) Bias due to missing data; 6) Bias in measurement of outcomes; and 7) Bias in selection of the reported result. Each dimension was evaluated as low risk, moderate risk, serious risk, critical risk, or no information. After summarizing these seven dimensions, the final risk level of the study was categorized as low risk (The study is judged to be at low risk of bias for all domains), moderate risk (The study is judged to be at low or moderate risk of bias for all domains), serious risk (The study is judged to be at serious risk of bias in at least one domain, but not at critical risk of bias in any domain), critical risk (The study is judged to be at critical risk of bias in at least one domain), or no information (There is no clear indication that the study is at serious or critical risk of bias and there is a lack of information in one or more key domains of bias). Following the assessment, it was independently reviewed by other authors.
Statistical analysis
This study used the Cochrane Collaborative Review Manager 5.4 software for conducting meta-analysis. For dichotomous variables, odds ratios (OR) were calculated and presented with 95% confidence intervals (CI). For continuous variables, weighted mean differences (WMD) were computed and presented with 95% CI. The heterogeneity among studies was assessed using the Q-test and I2-test, where I2 ≤ 50% indicated mild heterogeneity, ≤ 75% indicated moderate heterogeneity, and > 75% indicated high heterogeneity. A significance level of P < 0.05 was considered statistically significant. Due to inherent clinical heterogeneity in the data, a random-effects model was employed in all meta-analyses.
Subgroup analysis
If the extracted study data were stratified based on the relevant content, then subgroup analysis was conducted according to the stratification. If the included study data did not provide relevant content, subgroup analysis was not performed.
Publication bias
Egger’s test was used to detect publication bias and small-study effects of included studies.
| Results | ▴Top |
We initially retrieved 1,389 articles from the database. After excluding duplicates and non-English articles, we assessed whether the literature contained the necessary content for our study based on titles and abstracts. If titles and abstracts were not sufficient to determine compliance with our inclusion and exclusion criteria, we read the full text before making a decision. After excluding non-research articles (e.g., reviews, case reports/case series, and conference papers), meta-analyses, irrelevant studies, and non-comparative studies, there were nine articles comprising case-control studies with both LPN and LRN cohorts. Among these, one article did not provide separate data for laparoscopic surgery patients and open surgery patients within the cohorts [8], making it unable to provide the patient cohort data necessary for our study. Therefore, that article was excluded. Subsequently, we screened the references of studies comparing LPN and LRN cohorts and identified an article that met our criteria [9]. In the end, nine studies were included in this meta-analysis (Fig. 1).
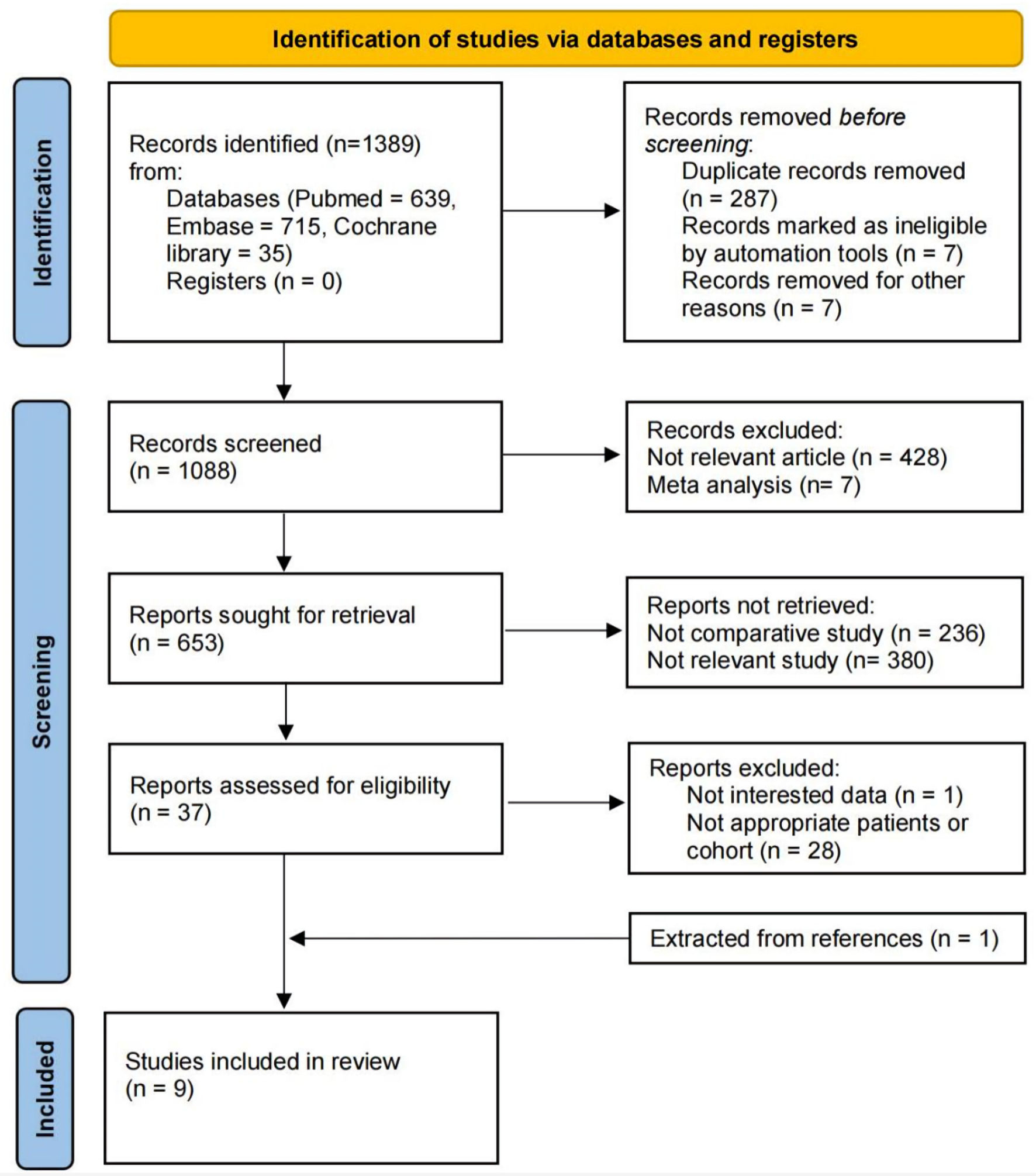 Click for large image | Figure 1. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2020 flow diagram for the systematic review. |
Baseline characteristics
The nine studies included in this meta-analysis were all single-center retrospective case-control studies published between 2009 and 2023 [9-17]; their patient data were sourced from the respective medical center databases, with two studies using propensity score matching [13, 15]. The total of 1,303 patients included in the meta-analysis (529 in the LPN group and 774 in the LRN group) originated from China (926 patients), the United States (348 patients), and Israel (29 patients). Baseline characteristics of patients from each study are shown in Table 1 [9-17].
 Click to view | Table 1. The Baseline Characteristics of Included Studies |
There was no significant heterogeneity in the baseline characteristics between the LPN and LRN cohorts in these nine studies (I2 ≤ 50%). There were no significant differences between the LPN and LRN groups in terms of age (P = 0.91), BMI (P = 0.72), proportion of males (P = 0.48), proportion of right renal tumors (P = 0.88), cT1b stage (P = 0.50), preoperative eGFR (P = 0.33), and the number of preoperative CKD cases (P = 0.66), with P < 0.05 considered statistically significant for differences (Table 2).
 Click to view | Table 2. The Heterogeneity Test for Baseline Characteristics |
Assessment of quality
Given that the included studies were retrospective case-control studies, we performed quality assessment of the included literature using the ROBINS-I tool. This tool assesses the quality of non-randomized controlled trials from seven dimensions, and the overall risk level is expressed as low, moderate, serious, or critical. Among the nine articles included in this study, seven were assessed as having a moderate risk, whereas two articles were considered to have a serious risk due to the potential for significant bias resulting from missing data (Table 3) [9-17].
 Click to view | Table 3. The Risk of Bias Assessment of Each Study by Using the ROBINS-I Tool |
Outcome analysis
Perioperative outcomes
Figure 2 presents a comparative analysis of perioperative outcomes between LPN and LRN groups across multiple studies. In six studies comprising 909 patients (422 LPN, 487 LRN), LPN exhibited longer surgery times by 12.86 min (95% CI (2.09, 23.62), P = 0.02). Furthermore, pooling data from five studies involving 659 patients indicated that LPN was associated with higher blood loss by 67.28 mL (95% CI (17.33, 117.23), P = 0.008) (Fig. 2b). The presence of high heterogeneity (surgery time: Chi2 = 18.39, I2 = 73%, P = 0.003; intraoperative blood loss: Chi2 = 35.20, I2 = 89%, P < 0.00001) underscores diverse study results, necessitating cautious interpretation.
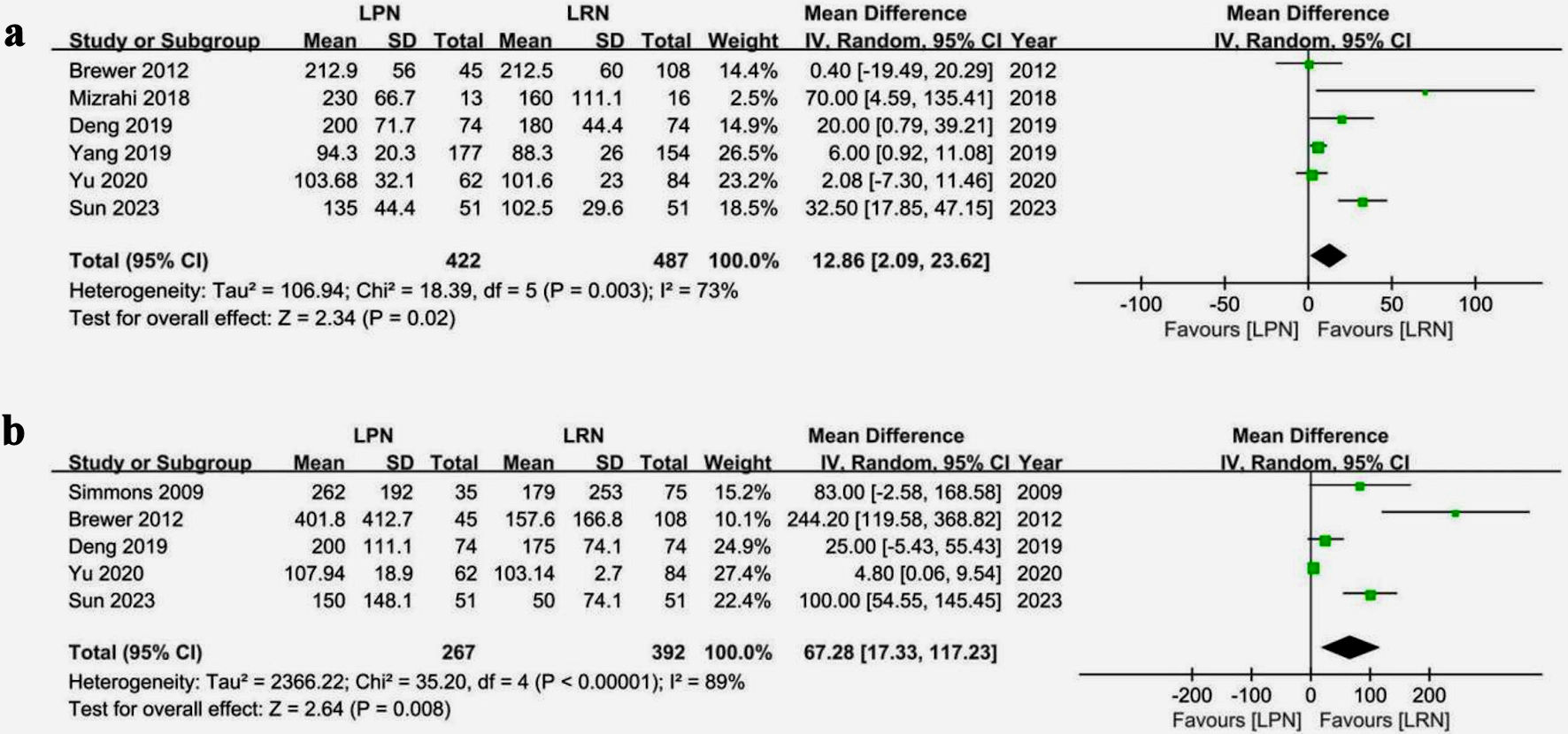 Click for large image | Figure 2. Forest plots of perioperative outcomes for LPN vs. LRN. (a) Operative time. (b) Intraoperative blood loss. LPN: laparoscopic partial nephrectomy; LRN: laparoscopic radical nephrectomy; CI: confidence interval; SD: standard deviation. |
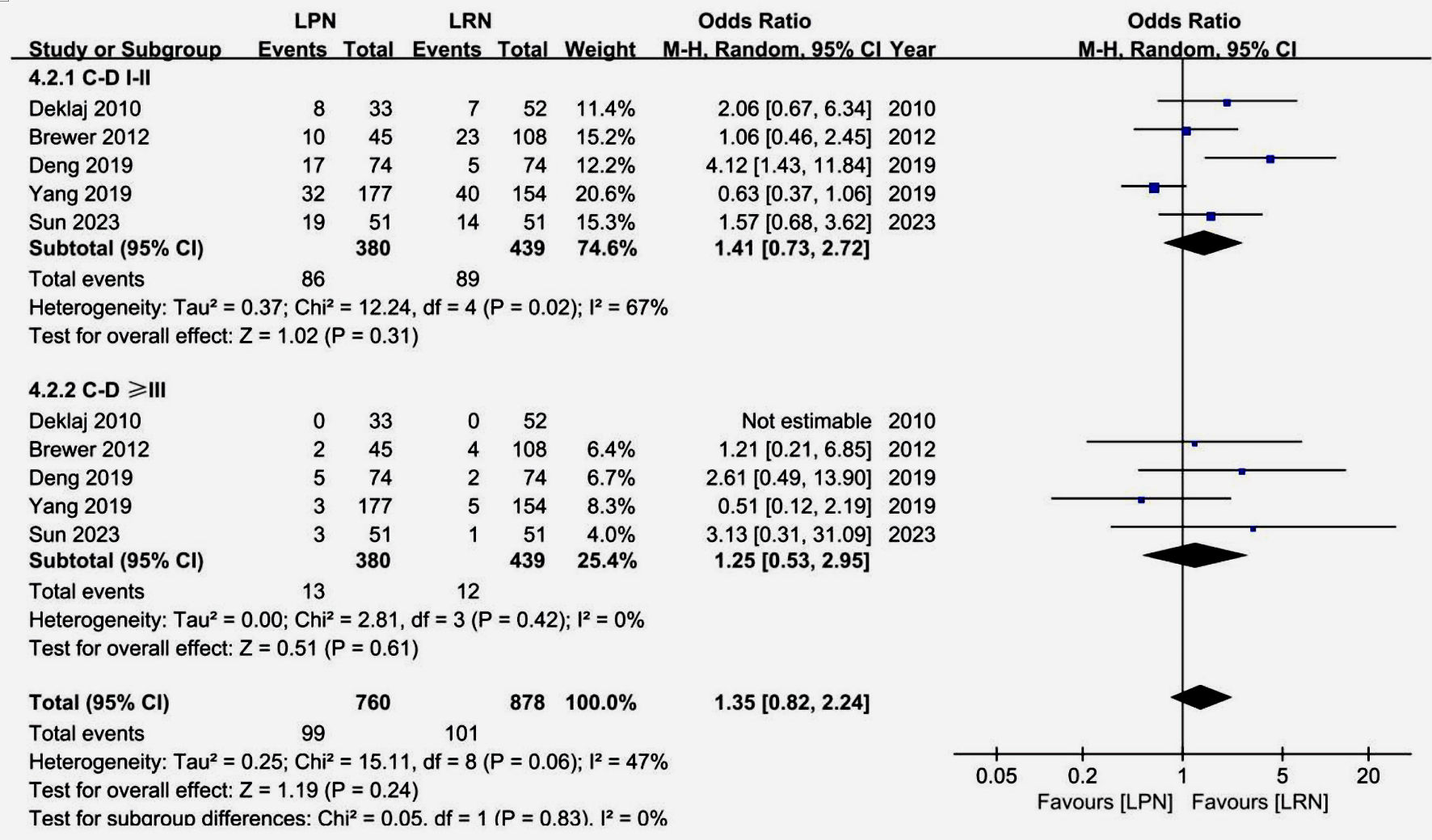 Click for large image | Figure 3. Forest plot of postoperative complications graded by Clavien-Dindo system. LPN: laparoscopic partial nephrectomy; LRN: laparoscopic radical nephrectomy; CI: confidence interval. |
Perioperative complications
Figure 3 undertakes an examination of perioperative complications within the context of LPN versus LRN groups. Utilizing the Clavien-Dindo system, the analysis reveals no statistically significant differences in complication rates between the two groups, whether classified as grade I - II (OR: 1.41, 95% CI: (0.73, 2.72), P = 0.31) or ≥ grade III (OR: 1.25, 95% CI (0.53, 2.95), P = 0.61). Moreover, the overall incidence of complications demonstrates similarity (OR: 1.35, 95% CI (0.82, 2.24), P = 0.24). While moderate heterogeneity is observed in grade I - II complications (Chi2 = 12.24, I2 = 67%, P = 0.02), it remains minimal or non-significant in other facets of the analysis.
Renal function outcomes
Figure 4 compares the changes in renal function post-surgery between the LPN and LRN groups. Across eight studies involving 1,274 patients, the LPN group exhibited a smaller decline in eGFR (ranging from 1.7 to 13.1 mL/min) compared to the LRN group (ranging from 16.9 to 32.91 mL/min), with a significant difference in decline favoring LPN (WMD 13.85 mL, 95% CI (10.05, 17.65), P < 0.00001) (Fig. 4a). Among 929 patients from six studies, a lower proportion of patients in the LPN group (40 out of 415) developed CKD (GFR < 60 mL/min) postoperatively compared to the LRN group (141 out of 514), indicating a significantly reduced incidence of postoperative CKD in the LPN group (OR: 0.23, 95% CI (0.10, 0.52), P = 0.0004) (Fig. 4b). Moderate heterogeneity was observed among the studies regarding both eGFR decline (Chi2 = 17.50, I2 = 60%, P = 0.01) and CKD incidence increases (Chi2 = 13.19, I2 = 62%, P = 0.02).
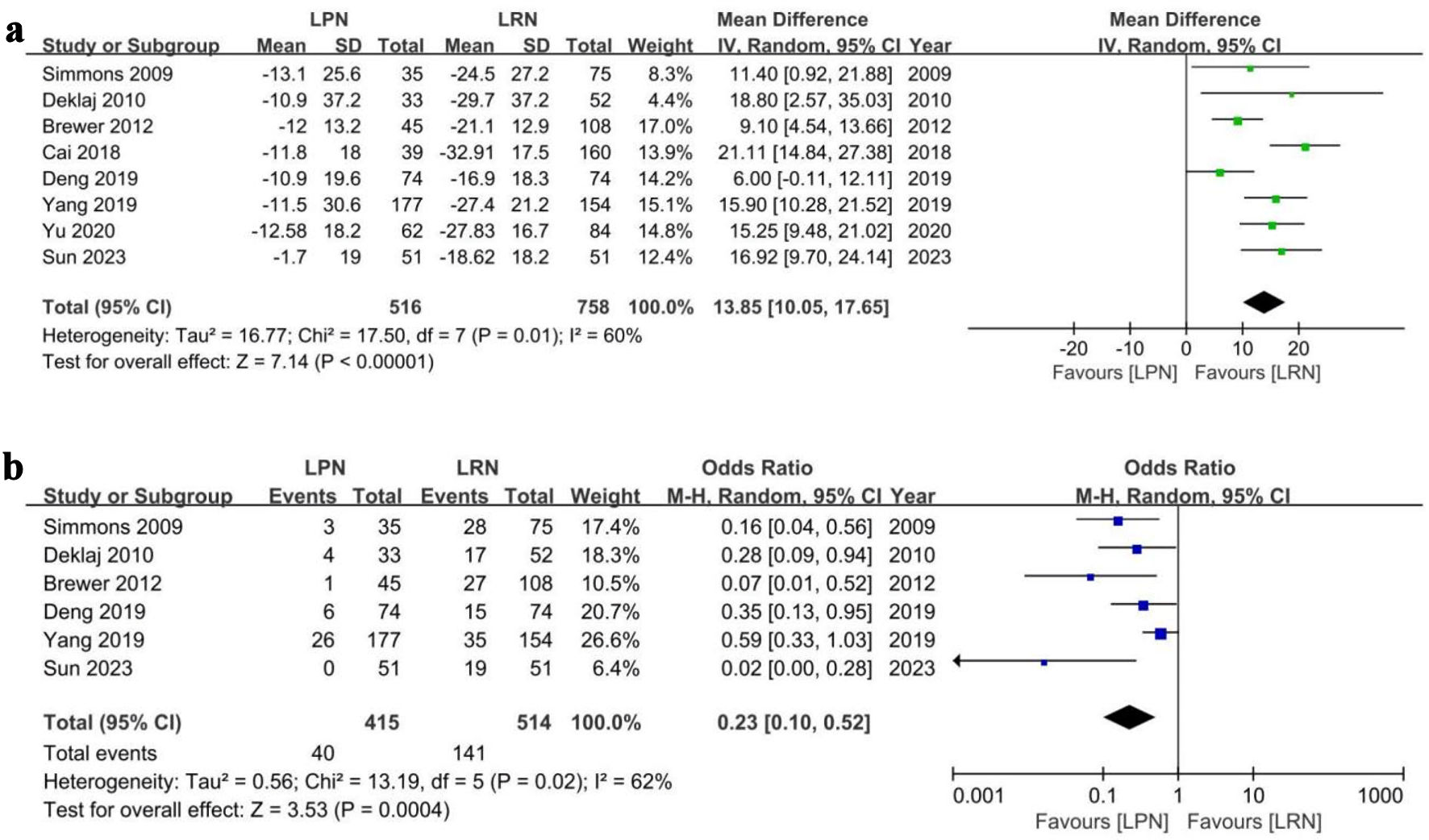 Click for large image | Figure 4. Forest plots of renal function outcomes for LPN vs LRN. (a) eGFR decline. (b) CKD increase. LPN: laparoscopic partial nephrectomy; LRN: laparoscopic radical nephrectomy; CI: confidence interval; SD: standard deviation. |
Oncological outcomes
Figure 5 presents the oncological outcomes from the studies. Data from six studies involving 887 patients indicated a slightly higher, albeit statistically insignificant, tumor recurrence rate (including local recurrence and distant metastasis) in the LPN group compared to LRN (OR: 1.06, 95% CI (0.42, 2.67), P = 0.91), with moderate study heterogeneity (Chi2 = 11.00, I2 = 55%, P = 0.05). CSM rates from three studies including 640 patients were significantly lower in LPN than LRN (OR: 0.40, 95% CI (0.20, 0.79), P = 0.008). OM rates did not differ significantly between the groups (OR: 0.91, 95% CI (0.24, 3.41), P = 0.89). Heterogeneity was low for CSM (Chi2 = 1.11, I2 = 0%, P = 0.58) and moderate for OM (Chi2 = 5.61, I2 = 64%, P = 0.06) (Fig. 5).
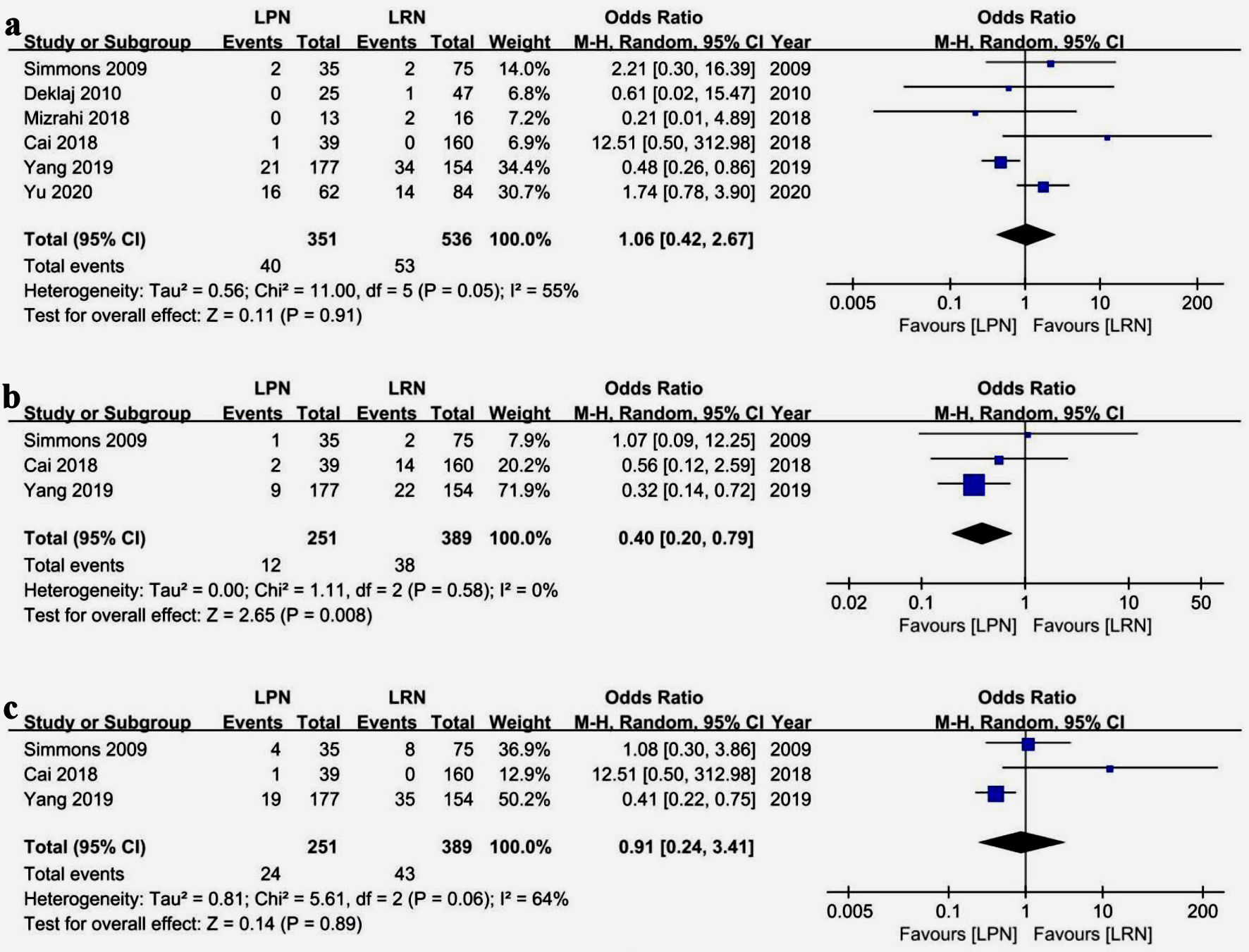 Click for large image | Figure 5. Forest plots of oncological outcomes for LPN vs. LRN. (a) Tumor recurrence (including local recurrence and distant metastasis). (b) Cancer-specific mortality. (c) Overall mortality. LPN: laparoscopic partial nephrectomy; LRN: laparoscopic radical nephrectomy; CI: confidence interval. |
Heterogeneity
After using the ROBINS-I tool to assess the quality of the literature, it was found that among the nine included studies, seven were of moderate quality and two were of lower quality. In the results of the meta-analysis, most outcomes showed a moderate-to-low degree of heterogeneity, whereas some outcomes showed a high degree of heterogeneity (such as operative time and intraoperative blood loss).
Sensitivity analysis
To ensure the robustness of our study and identify potential sources of heterogeneity, we conducted sensitivity analyses by systematically excluding one study at a time from the meta-analysis. This approach allowed us to assess the impact on both statistical significance and study heterogeneity, and it is not applicable to analyses comprising three or fewer studies. Our sensitivity analysis, which focused on key outcomes such as intraoperative blood loss, ≥ grade III postoperative complication rate, postoperative eGFR decline, and CKD incidence, reaffirmed the reliability of these findings, as evidenced by the absence of significant shifts in effect size, significance level, or heterogeneity. Following the exclusion of a single study, heterogeneity related to tumor recurrence was completely eliminated (heterogeneity I2: 55% to 0%), maintaining a consistent effect size. However, analyses pertaining to operative time and grade I - II postoperative complication rate exhibited considerable variability, raising concerns regarding the reliability of these results (Supplementary Material 2, www.wjon.org).
Publication bias
We utilized Egger’s test (considering P < 0.05 as statistically significant) to detecting publication bias. The result illustrates that for six effect sizes - surgery time, ≥ grade III postoperative complications, eGFR decline, the tumor recurrence rate, the CSM, and the OM - the intercept P values and slope P values all exceeded 0.05, indicating no significant publication bias. However, for intraoperative blood loss and grade I - II postoperative complications, intercept P values suggested potential bias (P = 0.027 and P = 0.047, respectively), despite nonsignificant slopes (P = 0.539 and P = 0.071, respectively), suggesting possible publication bias with a low probability of small-study effects. The intercept P values for overall postoperative complications and the increased postoperative incidence of CKD were both < 0.05, and the slope P values were close to 0.05, indicating a higher likelihood of publication bias and small-study effects for these two conclusions. The presence of random variability in Egger’s test and the small sample sizes for certain conclusions could impact accuracy. Therefore, while Egger’s test did not conclusively indicate publication bias for most measured effects, the potential bias for intraoperative blood loss and grade I - II postoperative complications, coupled with a significant risk of bias and small-study effects for overall postoperative complications and CKD incidence post-operation, may undermine the reliability of these findings (Table 4).
 Click to view | Table 4. The Egger’s Test for Effect Sizes |
| Discussion | ▴Top |
Several published meta-analyses on the efficacy differences between PN and RN in treating large renal tumors indicate that, although PN requires a longer operation time, incurs more intraoperative bleeding, and presents a higher risk of postoperative complications compared to RN, PN significantly outperforms RN in preserving renal function. In terms of oncological outcomes, the tumor recurrence rate of PN is not higher than that of RN. However, further meta-analyses on survival data for PN and RN are insufficient to determine which surgical method is superior concerning various survival and mortality rates (Table 5) [18-23]. These meta-analyses have synthesized a broad range of comparative studies on PN and RN, preliminarily exploring the efficacy differences between the two surgical methods in treating renal tumors and drawing some practically significant conclusions. Nonetheless, these meta-analyses did not differentiate specific surgical techniques (such as open surgery, laparoscopic surgery, and robotic-assisted surgery), which introduces a degree of bias to the study’s conclusions [18-23]. Therefore, in this study, we selected comparative studies including LPN and LRN for meta-analysis to obtain more reliable conclusions. Nine studies related to the treatment of large-volume renal tumors using LPN and LRN were included in this meta-analysis. The overall quality of the included literature was moderate. After conducting meta-analyses of perioperative outcomes, renal function outcomes, and oncologic outcomes of each study, most conclusions were found to have a low risk of bias and good evidence quality. Few conclusions exhibited high heterogeneity or publication bias, leading to decreased credibility of the results.
 Click to view | Table 5. Relevant Meta-Analysis Comparing PN and RN |
In the strategic planning of surgical interventions for renal tumors, determining tumor size plays a pivotal role in selecting between PN for smaller tumors and RN for larger ones. The feasibility of laparoscopic surgery depends on the available abdominal space, and for larger tumors, open surgery may be imperative. Nevertheless, it is essential to acknowledge the presence of selection bias stemming from the retrospective nature of the included studies and the assessment of suitability for laparoscopic surgery. Factors such as the study period (2003 - 2017) and variations in surgical expertise across different medical centers contribute to the decision between LPN and LRN. Additionally, considerations of tumor location and complexity, evaluated through tools like the RENAL score [24] and SARR scores [25], significantly influence the chosen surgical approach, with more intricate tumors being less amenable to PN. Despite included studies hinting at LRN potentially being superior to LPN for large tumors, the evidence is inconclusive, emphasizing the critical role of evaluating the proficiency of the surgical center and the complexity of the tumor for future analyses. Notably, limited reporting of tumor complexity scores in a subset of studies in our meta-analysis constrains subgroup analysis, underscoring the imperative for further research that extends beyond tumor volume and encompasses various factors in the diagnosis and treatment of large-volume renal tumors [26-28].
This study revealed that compared to LRN, LPN is associated with longer surgery times (P = 0.02) and increased blood loss (P = 0.008). Subgroup analysis indicated higher rates of both grade I - II (P = 0.31) and ≥ grade III (P = 0.61) postoperative complications in LPN. After heterogeneity testing and sensitivity analysis, the more reliable conclusion was that the rate of ≥ grade III complications was higher with LPN than with LRN. Compared to LRN, LPN requires more time in several key steps (clamping renal vessels, excising renal tumors, and suturing the renal incision), and these critical steps have certain technical thresholds [29], resulting in a longer learning curve for LPN under similar conditions. However, with the increasing maturity of laparoscopic techniques and the introduction of surgical robots, both the learning curve and surgical time for LPN and LRN are gradually decreasing [30-32]. Common complications of LPN include renal incision bleeding, acute kidney injury, urinary leakage, abdominal infection, and urinary tract infection, with incidence rates ranging from 9% to 30% [33, 34]. Among these, complications such as incision bleeding, acute kidney injury, and urinary leakage are closely related to the critical steps of LPN. Improper handling during surgery can lead to severe consequences, often requiring secondary surgery or intensive care. Proficient mastery of LPN surgical techniques, reducing the intraoperative warm ischemia time, and shortening the surgical time can significantly prevent these complications [34, 35].
The greatest advantage of LPN over LRN lies in the preservation of renal units, which can reduce the risk of long-term renal dysfunction and cardiovascular events in patients after the operation [36, 37]. Our results reveal that the postoperative eGFR in the LRN group decreased by an additional 13.85 mL/min (95% CI (10.05, 17.65), P < 0.00001) compared to the LPN group. The number of cases with postoperative onset of CKD was significantly smaller in the LPN group than in the LRN group (OR: 0.23, 95% CI (0.10, 0.52), P = 0.0004). Compared to RN, PN significantly preserves renal function [37, 38] and reduces the risk of postoperative CKD [39]. Additionally, PN diminishes the risks of cardiovascular and metabolic diseases by better preserving endocrine function. Weight et al have reported that the renal function loss caused by RN leads to a 25% increase in the risk of postoperative cardiovascular disease-related mortality [40], and this risk is particularly evident in elderly patients with renal tumors [41]. The foundation underlying the excellent protective effect of PN on renal function is excellent surgical technique [42, 43]. In terms of PN surgery, intraoperative interruption of renal blood flow poses potential risks of damage to healthy renal units [44, 45]. Although it is generally recommended to limit warm ischemia time within 20 - 30 min, there is no absolute safe threshold, and each minute of warm ischemia can harm renal function [46, 47]. Therefore, techniques such as selective arterial clamping and bloodless clamping are recommended to mitigate renal ischemia [48, 49], particularly advantageous for large renal tumors. Our findings advocate for the efficacy of LPN in preserving renal function in large tumors (> 4 cm), emphasizing the importance of controlling ischemia time and considering zero-ischemia techniques [50, 51].
We compared tumor recurrence rates, the OM, and the CSM in oncological outcomes. We found that the tumor recurrence rate was similar in the LPN group (including local recurrence and distant metastasis) than in the LRN group (OR: 1.06, 95% CI (0.42, 2.67)), but the difference between the two groups was not statistically significant (P = 0.91). The OM was lower in the LPN group than in the LRN group (OR: 0.91 (0.24, 3.41), P = 0.89), and the CSM was significantly lower in the LPN group than in the LRN group (OR: 0.40, 95% CI (0.20, 0.79), P = 0.008). There has been a long-standing controversy regarding the superiority or inferiority of PN and RN in oncological outcomes. Despite the possibility of positive surgical margins after PN, most studies suggest that positive margins after PN do not increase the risk of local tumor recurrence or metastasis [52-54]. Tumor recurrence and metastasis after PN are often associated with the higher pathological grade of the tumor itself [55, 56], a factor similar to the risk factors for recurrence and metastasis after RN [57]. Numerous studies have been conducted on the postoperative survival outcomes of renal tumors, especially large-volume renal tumors. The propensity score-matched study by Simone et al revealed no significant disparities between the two cohorts of cT1-cT2N0M0 renal tumor patients undergoing either minimally invasive partial nephrectomy (MIPN) or minimally invasive radical nephrectomy (MIRN), concerning metastasis-free survival (P = 0.811), local recurrence-free survival (P = 0.283), overall survival (OS) (P = 0.419), and cancer-specific survival (CSS) (P = 0.907) [58]. Saint Aubert et al found no significant differences in OS, recurrence-free survival, and recurrence-specific survival between patients with cT2-stage renal tumors undergoing PN or RN [59]. Similarly, the findings of Ristau et al also suggest that PN does not provide a survival advantage over RN in patients with large-volume renal tumors [60]. Conversely, the retrospective study by Janssen et al found that the long-term OS and CSS of patients with renal tumors ≥ 7 cm were significantly longer in the PN group than in the RN group [61]. In summary, regarding oncological outcomes, we found no significant difference between the LPN and LRN groups in terms of tumor recurrence rate and OM. Conversely, the CSM was significantly better in the LPN group than in the LRN group. However, due to the limited number of included studies, there is a potential for bias in this regard.
Our study has significant limitations. First, all included studies were retrospective and of moderate overall quality, which may introduce selection bias, confounding bias, and observer bias. Second, we summarized and analyzed relevant studies based on tumor size without considering the impact of tumor complexity on the study results. In addition, due to the lack of relevant data in the literature, we were unable to conduct corresponding subgroup analyses. Third, the variability in the length of follow-up time limited the comparison of oncological outcomes. Finally, for some outcomes, such as intraoperative complications, the OM, and the CSM, only a few studies provided the corresponding data, thus reducing the credibility of the results.
Conclusions
In the treatment of localized, large renal tumors (cT1b-cT2N0M0), our study revealed that LPN entailed longer surgery times and greater intraoperative blood loss compared to LRN, with LPN exhibiting a higher rate of significant postoperative complications. However, LPN demonstrated a distinct advantage in preserving renal function post-surgery. Tumor recurrence rates post-operation were similar between the two procedures, and while overall mortality was comparable, CSM was notably lower in the LPN group. However, these conclusions are derived from a limited set of retrospective studies, suggesting a moderate confidence level in these findings. There is a call for future research with more robust designs and longer follow-up to thoroughly assess the comparative outcomes of these surgical methods for large renal tumors.
| Supplementary Material | ▴Top |
Suppl 1. Search history.
Suppl 2. Leave-one-out sensitivity analysis for meta-analysis results.
Acknowledgments
None to declare.
Financial Disclosure
This work was supported by the National Natural Science Foundation of China (No. 82060464) and the Yunnan Science and Technology Department and Kunming Medical University Special Fund (Grant No. 202001AY070001-148).
Conflict of Interest
All authors have no conflict of interest to disclose.
Informed Consent
Not applicable.
Author Contributions
Bao Nan Dong: data curation, formal analysis, writing - original draft preparation. Jie Song: data curation, formal analysis. Wen Li Yang: data curation, formal analysis. Hui Zhan: funding acquisition, conceptualization, supervision, writing - review and editing. Ting Luan: funding acquisition, conceptualization, writing - review and editing. Jian Song Wang: funding acquisition and supervision. All authors read and approved the final manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
LPN: laparoscopic partial nephrectomy; LRN: laparoscopic radical nephrectomy; PN: partial nephrectomy; RN: radical nephrectomy; C-D: Clavien-Dindo; eGFR: estimated glomerular filtration rate; OR: odds ratio; CI: confidence interval; WMD: weighted mean differences; PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses; MPN: minimally invasive partial nephrectomy; MRN: minimally invasive radical nephrectomy; RLPN: robotic-assisted laparoscopic partial nephrectomy; RLRN: Robotic-assisted laparoscopic radical nephrectomy; BMI: body mass index; R/L: right/left; CKD: chronic kidney disease; NA: not available; CSM: cancer-specific mortality; OM: overall mortality
| References | ▴Top |
- Delahunt B, Eble JN, Samaratunga H, Thunders M, Yaxley JW, Egevad L. Staging of renal cell carcinoma: current progress and potential advances. Pathology. 2021;53(1):120-128.
doi pubmed - Patel HD, Gupta M, Joice GA, Srivastava A, Alam R, Allaf ME, Pierorazio PM. Clinical stage migration and survival for renal cell carcinoma in the United States. Eur Urol Oncol. 2019;2(4):343-348.
doi pubmed - Banegas MP, Harlan LC, Mann B, Yabroff KR. Toward greater adoption of minimally invasive and nephron-sparing surgical techniques for renal cell cancer in the United States. Urol Oncol. 2016;34(10):433.e9-433.e17.
doi pubmed pmc - Patard JJ, Shvarts O, Lam JS, Pantuck AJ, Kim HL, Ficarra V, Cindolo L, et al. Safety and efficacy of partial nephrectomy for all T1 tumors based on an international multicenter experience. J Urol. 2004;171(6 Pt 1):2181-2185.
doi pubmed - Talenfeld AD, Gennarelli RL, Elkin EB, Atoria CL, Durack JC, Huang WC, Kwan SW. Percutaneous ablation versus partial and radical nephrectomy for T1a renal cancer: a population-based analysis. Ann Intern Med. 2018;169(2):69-77.
doi pubmed pmc - Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
doi pubmed pmc - Sterne JA, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M, Henry D, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
doi pubmed pmc - Thompson RH, Siddiqui S, Lohse CM, Leibovich BC, Russo P, Blute ML. Partial versus radical nephrectomy for 4 to 7 cm renal cortical tumors. J Urol. 2009;182(6):2601-2606.
doi pubmed pmc - Brewer K, O'Malley RL, Hayn M, Safwat MW, Kim H, Underwood W, 3rd, Schwaab T. Perioperative and renal function outcomes of minimally invasive partial nephrectomy for T1b and T2a kidney tumors. J Endourol. 2012;26(3):244-248.
doi pubmed - Simmons MN, Weight CJ, Gill IS. Laparoscopic radical versus partial nephrectomy for tumors >4 cm: intermediate-term oncologic and functional outcomes. Urology. 2009;73(5):1077-1082.
doi pubmed - Deklaj T, Lifshitz DA, Shikanov SA, Katz MH, Zorn KC, Shalhav AL. Laparoscopic radical versus laparoscopic partial nephrectomy for clinical T1bN0M0 renal tumors: comparison of perioperative, pathological, and functional outcomes. J Endourol. 2010;24(10):1603-1607.
doi pubmed - Rinott Mizrahi G, Freifeld Y, Klein I, Boyarsky L, Zreik R, Orlin I, Friedman B, et al. Comparison of partial and radical laparascopic nephrectomy: perioperative and oncologic outcomes for clinical T2 renal cell carcinoma. J Endourol. 2018;32(10):950-954.
doi pubmed - Deng W, Zhou Z, Zhong J, Li J, Liu X, Chen L, Zhu J, et al. Retroperitoneal laparoscopic partial versus radical nephrectomy for large (>/= 4 cm) and anatomically complex renal tumors: A propensity score matching study. Eur J Surg Oncol. 2020;46(7):1360-1365.
doi pubmed - Yang F, Zhou Q, Xing N. Comparison of survival and renal function between partial and radical laparoscopic nephrectomy for T1b renal cell carcinoma. J Cancer Res Clin Oncol. 2020;146(1):261-272.
doi pubmed - Sun ZJ, Liu F, Wei HB, Zhang DH. Laparoscopic partial versus radical nephrectomy for localized renal cell carcinoma over 4 cm. J Cancer Res Clin Oncol. 2023;149(20):17837-17848.
doi pubmed pmc - Cai Y, Li HZ, Zhang YS. Comparison of Partial and Radical Laparascopic Nephrectomy: Long-Term Outcomes for Clinical T1b Renal Cell Carcinoma. Urol J. 2018;15(2):16-20.
doi pubmed - Yu K, Liu M, Xie Z, Yu Z, Liu S. Comparison of efficacy and long-term survival of laparoscopic radical nephrectomy with partial nephrectomy in the treatment of patients with early renal cell carcinoma Running title: laparoscopic radical nephrectomy. J BUON. 2020;25(2):1155-1160.
pubmed - Jiang YL, Peng CX, Wang HZ, Qian LJ. Comparison of the long-term follow-up and perioperative outcomes of partial nephrectomy and radical nephrectomy for 4 cm to 7 cm renal cell carcinoma: a systematic review and meta-analysis. BMC Urol. 2019;19(1):48.
doi pubmed pmc - Zhang Y, Long G, Shang H, Ding B, Sun G, Ouyang W, Liu M, et al. Comparison of the oncological, perioperative and functional outcomes of partial nephrectomy versus radical nephrectomy for clinical T1b renal cell carcinoma: A systematic review and meta-analysis of retrospective studies. Asian J Urol. 2021;8(1):117-125.
doi pubmed pmc - Mir MC, Derweesh I, Porpiglia F, Zargar H, Mottrie A, Autorino R. Partial Nephrectomy Versus Radical Nephrectomy for Clinical T1b and T2 Renal Tumors: A Systematic Review and Meta-analysis of Comparative Studies. Eur Urol. 2017;71(4):606-617.
doi pubmed - Huang R, Zhang C, Wang X, Hu H. Partial nephrectomy versus radical nephrectomy for clinical T2 or higher stage renal tumors: a systematic review and meta-analysis. Front Oncol. 2021;11:680842.
doi pubmed pmc - Li J, Zhang Y, Teng Z, Han Z. Partial nephrectomy versus radical nephrectomy for cT2 or greater renal tumors: a systematic review and meta-analysis. Minerva Urol Nefrol. 2019;71(5):435-444.
doi pubmed - Deng W, Chen L, Wang Y, Liu X, Wang G, Fu B. Partial nephrectomy versus radical nephrectomy for large (>/= 7 cm) renal tumors: A systematic review and meta-analysis. Urol Oncol. 2019;37(4):263-272.
doi pubmed - Kutikov A, Uzzo RG. The R.E.N.A.L. nephrometry score: a comprehensive standardized system for quantitating renal tumor size, location and depth. J Urol. 2009;182(3):844-853.
doi pubmed - Tannus M, Goldman SM, Andreoni C. Practical and intuitive surgical approach renal ranking to predict outcomes in the management of renal tumors: a novel score tool. J Endourol. 2014;28(4):487-492.
doi pubmed - Campbell SC, Clark PE, Chang SS, Karam JA, Souter L, Uzzo RG. Renal mass and localized renal cancer: evaluation, management, and follow-up: AUA guideline: Part I. J Urol. 2021;206(2):199-208.
doi pubmed - Ljungberg B, Albiges L, Abu-Ghanem Y, Bedke J, Capitanio U, Dabestani S, Fernandez-Pello S, et al. European Association of Urology Guidelines on Renal Cell Carcinoma: the 2022 update. Eur Urol. 2022;82(4):399-410.
doi pubmed - Motzer RJ, Jonasch E, Agarwal N, Alva A, Baine M, Beckermann K, Carlo MI, et al. Kidney Cancer, Version 3.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2022;20(1):71-90.
doi pubmed pmc - Zhao PT, Richstone L, Kavoussi LR. Laparoscopic partial nephrectomy. Int J Surg. 2016;36(Pt C):548-553.
doi pubmed - Pandey A, Mandal S, Das MK, Nayak P. Laparoscopic Radical Nephrectomy in the Current Era: Technical Difficulties, Troubleshoots, a Guide to the Apprentice, and the Current Learning Curve. South Asian J Cancer. 2023;12(2):141-147.
doi pubmed pmc - Hanzly M, Frederick A, Creighton T, Atwood K, Mehedint D, Kauffman EC, Kim HL, et al. Learning curves for robot-assisted and laparoscopic partial nephrectomy. J Endourol. 2015;29(3):297-303.
doi pubmed - Patel HD, Mullins JK, Pierorazio PM, Jayram G, Cohen JE, Matlaga BR, Allaf ME. Trends in renal surgery: robotic technology is associated with increased use of partial nephrectomy. J Urol. 2013;189(4):1229-1235.
doi pubmed - Zimmermann R, Janetschek G. Complications of laparoscopic partial nephrectomy. World J Urol. 2008;26(6):531-537.
doi pubmed - Sharma E, Chally PR, Santhosh S, Ratkal JM. Complications and renal functional deterioration in patients with co-morbidities following laparoscopic partial nephrectomy. Afr J Urol. 2016;22(3):162-167.
doi - Jimenez-Romero ME, Moreno-Cortes JC, Canelon-Castillo EY, Diez-Farto S, Santotoribio JD. Predictive factors of renal function in partial laparoscopic nephrectomy in patients with a kidney tumor. Curr Urol. 2019;13(3):150-156.
doi pubmed pmc - Li M, Cheng L, Zhang H, Ma L, Wang Y, Niu W, Liu Z, et al. Laparoscopic and Robotic-Assisted Partial Nephrectomy: An Overview of Hot Issues. Urol Int. 2020;104(9-10):669-677.
doi pubmed - Li L, Lau WL, Rhee CM, Harley K, Kovesdy CP, Sim JJ, Jacobsen S, et al. Risk of chronic kidney disease after cancer nephrectomy. Nat Rev Nephrol. 2014;10(3):135-145.
doi pubmed - Patel HD, Pierorazio PM, Johnson MH, Sharma R, Iyoha E, Allaf ME, Bass EB, et al. Renal Functional Outcomes after Surgery, Ablation, and Active Surveillance of Localized Renal Tumors: A Systematic Review and Meta-Analysis. Clin J Am Soc Nephrol. 2017;12(7):1057-1069.
doi pubmed pmc - Mukkamala A, He C, Weizer AZ, Hafez KS, Miller DC, Montgomery JS, Bitzer M, et al. Long-term renal functional outcomes of minimally invasive partial nephrectomy for renal cell carcinoma. Urol Oncol. 2014;32(8):1247-1251.
doi pubmed - Weight CJ, Larson BT, Fergany AF, Gao T, Lane BR, Campbell SC, Kaouk JH, et al. Nephrectomy induced chronic renal insufficiency is associated with increased risk of cardiovascular death and death from any cause in patients with localized cT1b renal masses. J Urol. 2010;183(4):1317-1323.
doi pubmed - Chung JS, Son NH, Lee SE, Hong SK, Lee SC, Kwak C, Hong SH, et al. Overall survival and renal function after partial and radical nephrectomy among older patients with localised renal cell carcinoma: a propensity-matched multicentre study. Eur J Cancer. 2015;51(4):489-497.
doi pubmed - Kim WH, Yoon HK, Lee HJ. Acute kidney injury and long-term renal function after partial nephrectomy-is there a true association? Ann Transl Med. 2019;7(Suppl 6):S241.
doi pubmed pmc - Bravi CA, Vertosick E, Benfante N, Tin A, Sjoberg D, Hakimi AA, Touijer K, et al. Impact of Acute Kidney Injury and Its Duration on Long-term Renal Function After Partial Nephrectomy. Eur Urol. 2019;76(3):398-403.
doi pubmed pmc - Thompson RH, Lane BR, Lohse CM, Leibovich BC, Fergany A, Frank I, Gill IS, et al. Renal function after partial nephrectomy: effect of warm ischemia relative to quantity and quality of preserved kidney. Urology. 2012;79(2):356-360.
doi pubmed - Choi JD, Park JW, Lee SY, Jeong BC, Jeon SS, Lee HM, Choi HY, et al. Does prolonged warm ischemia after partial nephrectomy under pneumoperitoneum cause irreversible damage to the affected kidney? J Urol. 2012;187(3):802-806.
doi pubmed - Thompson RH, Lane BR, Lohse CM, Leibovich BC, Fergany A, Frank I, Gill IS, et al. Every minute counts when the renal hilum is clamped during partial nephrectomy. Eur Urol. 2010;58(3):340-345.
doi pubmed - Patel AR, Eggener SE. Warm ischemia less than 30 minutes is not necessarily safe during partial nephrectomy: every minute matters. Urol Oncol. 2011;29(6):826-828.
doi pubmed - Martin GL, Warner JN, Nateras RN, Andrews PE, Humphreys MR, Castle EP. Comparison of total, selective, and nonarterial clamping techniques during laparoscopic and robot-assisted partial nephrectomy. J Endourol. 2012;26(2):152-156.
doi pubmed - Ukimura O, Nakamoto M, Gill IS. Three-dimensional reconstruction of renovascular-tumor anatomy to facilitate zero-ischemia partial nephrectomy. Eur Urol. 2012;61(1):211-217.
doi pubmed - Papalia R, Simone G, Ferriero M, Guaglianone S, Costantini M, Giannarelli D, Maini CL, et al. Laparoscopic and robotic partial nephrectomy without renal ischaemia for tumours larger than 4 cm: perioperative and functional outcomes. World J Urol. 2012;30(5):671-676.
doi pubmed - Simone G, Ferriero M, Papalia R, Costantini M, Guaglianone S, Gallucci M. Zero-ischemia minimally invasive partial nephrectomy. Curr Urol Rep. 2013;14(5):465-470.
doi pubmed - Marszalek M, Carini M, Chlosta P, Jeschke K, Kirkali Z, Knuchel R, Madersbacher S, et al. Positive surgical margins after nephron-sparing surgery. Eur Urol. 2012;61(4):757-763.
doi pubmed - Yossepowitch O, Thompson RH, Leibovich BC, Eggener SE, Pettus JA, Kwon ED, Herr HW, et al. Positive surgical margins at partial nephrectomy: predictors and oncological outcomes. J Urol. 2008;179(6):2158-2163.
doi pubmed pmc - Permpongkosol S, Colombo JR, Jr., Gill IS, Kavoussi LR. Positive surgical parenchymal margin after laparoscopic partial nephrectomy for renal cell carcinoma: oncological outcomes. J Urol. 2006;176(6 Pt 1):2401-2404.
doi pubmed - Takagi T, Yoshida K, Wada A, Kondo T, Fukuda H, Ishihara H, Kobayashi H, et al. Predictive factors for recurrence after partial nephrectomy for clinical T1 renal cell carcinoma: a retrospective study of 1227 cases from a single institution. Int J Clin Oncol. 2020;25(5):892-898.
doi pubmed - van der Mijn JC, Al Hussein Al Awamlh B, Islam Khan A, Posada-Calderon L, Oromendia C, Fainberg J, Alshak M, et al. Validation of risk factors for recurrence of renal cell carcinoma: Results from a large single-institution series. PLoS One. 2019;14(12):e0226285.
doi pubmed pmc - Yoo GS, Park W, Pyo H, Jeong BC, Jeon HG, Kang M, Seo SI, et al. Risk Factors and Patterns of Locoregional Recurrence after Radical Nephrectomy for Locally Advanced Renal Cell Carcinoma. Cancer Res Treat. 2022;54(1):218-225.
doi pubmed pmc - Simone G, Tuderti G, Anceschi U, Papalia R, Ferriero M, Misuraca L, Minisola F, et al. Oncological outcomes of minimally invasive partial versus minimally invasive radical nephrectomy for cT1-2/N0/M0 clear cell renal cell carcinoma: a propensity score-matched analysis. World J Urol. 2017;35(5):789-794.
doi pubmed - de Saint Aubert N, Audenet F, McCaig F, Delavaud C, Verkarre V, Le Guilchet T, Dariane C, et al. Nephron sparing surgery in tumours greater than 7cm. Prog Urol. 2018;28(6):336-343.
doi pubmed - Ristau BT, Handorf EA, Cahn DB, Kutikov A, Uzzo RG, Smaldone MC. Partial nephrectomy is not associated with an overall survival advantage over radical nephrectomy in elderly patients with stage Ib-II renal masses: An analysis of the national cancer data base. Cancer. 2018;124(19):3839-3848.
doi pubmed - Janssen MWW, Linxweiler J, Terwey S, Rugge S, Ohlmann CH, Becker F, Thomas C, et al. Survival outcomes in patients with large (≥7cm) clear cell renal cell carcinomas treated with nephron-sparing surgery versus radical nephrectomy: Results of a multicenter cohort with long-term follow-up. PLoS One. 2018;13(5):e0196427.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Oncology is published by Elmer Press Inc.


